堕胎是怀孕的结束,因为胚胎或胎儿在子宫外能够存活之前将其移除。[注1]自发发生的堕胎也称为流产。当采取刻意的措施来结束怀孕时,它被称为人工流产,或者更少的是“诱导流产”。堕胎一词通常用于表示只有人工流产。[1]胎儿可能在子宫外存活后的类似程序被称为“晚期终止妊娠”或不太准确的“晚期流产”。[2]
在法律允许的情况下,发达国家的堕胎是最安全的医学程序之一。[3] [4]现代方法使用药物或手术进行堕胎。[5]药物米非司酮联合前列腺素似乎与妊娠中期和孕中期的手术一样安全有效[5] [6]。最常见的手术技术包括扩张子宫颈和使用抽吸装置。[7]避孕药可以在堕胎后立即使用,例如避孕药或宫内避孕器。[6]如果合法安全地进行,人工流产不会增加长期精神或身体问题的风险。[8]相比之下,不安全的堕胎(由非熟练人员,危险设备或不卫生设施进行的堕胎)导致每年47,000人死亡和500万人入院。[8] [9]世界卫生组织建议所有妇女都能获得安全合法的堕胎。[10]
世界上每年约有5600万例堕胎,[11]其中约45%的堕胎不安全。[12] 2003年至2008年期间堕胎率几乎没有变化,[13]之前,随着计划生育和计划生育的增加,堕胎率下降了至少20年。[14]截至2008年,世界上40%的妇女可以在没有理由限制的情况下获得合法堕胎。[15]允许堕胎的国家对允许堕胎的晚期有不同的限制。[15]
从历史上看,已经尝试使用草药,尖锐工具,强力按摩或其他传统方法进行堕胎。[16]堕胎法和堕胎的文化或宗教观点在世界各地都不同。在某些地区,堕胎只在特定情况下是合法的,例如强奸,胎儿问题,贫困,妇女健康风险或乱伦。[17]在许多地方,关于堕胎的道德,伦理和法律问题存在很多争论。[18] [19]那些反对堕胎的人经常认为胚胎或胎儿是一个有生命权的人,所以他们可以比较堕胎和谋杀。[20] [21]那些赞成堕胎合法性的人常常认为女性有权决定自己的身体。[22]其他人则赞成将合法和无障碍堕胎作为一项公共卫生措施。[23]
目录
1 类型
1.1 诱导
1.2 自发性
2 方法
2.1 医疗
2.2 手术
2.3 人工流产
2.4 其他方法
3 安全
3.1 心理健康
3.2 不安全流产
3.3 活产
4 发病率
4.1 孕龄和方法
5 动机
5.1 个人
5.2 社会性
5.3 孕产妇和胎儿的健康
6 历史和宗教
7 社会与文化
7.1 堕胎辩论
7.2 现代堕胎法
7.3 性别选择性流产
7.4 反堕胎暴力
8 其他动物
9 参考
类型
诱发
人工流产可分为治疗性(根据妇女或胎儿的健康状况进行)或选择性(由于其他原因选择)。[24]
全世界每年大约有2.05亿人怀孕。超过三分之一是无意识的,大约五分之一是人工流产。[13] [25]大多数堕胎都是由于意外怀孕造成的。[26] [27]在英国,1%至2%的堕胎是由于胎儿的遗传问题而完成的。[8]怀孕可以通过多种方式故意中止。选择的方式通常取决于胚胎或胎儿的胎龄,随着妊娠的进展,胎龄会增加。[28] [29]由于合法性,地区可用性以及医生或女性的个人偏好,也可以选择特定程序。
获得人工流产的原因通常表征为治疗性或选择性。堕胎在医学上被称为治疗性堕胎,用于挽救孕妇的生命;防止伤害妇女的身心健康;终止妊娠,表明儿童的死亡或发病几率会大大增加;或选择性地减少胎儿数量,以减轻多胎妊娠相关的健康风险。[30] [31]堕胎在妇女非医疗原因的要求下进行时被称为选择性或自愿性堕胎。[31]由于“选择性手术”通常是指所有预定的手术,无论是否在医学上是必要的,因此有时会出现“选择性”一词的混淆。[32]
自发
主要文章:流产
自然流产,也称为流产,是在妊娠第24周之前无意中驱逐胚胎或胎儿。[33]妊娠37周结束导致活产婴儿的妊娠被称为“早产”。[34]当胎儿在生存后或分娩过程中在子宫内死亡时,通常称为“死产”。[35]早产和死产通常不被认为是流产,尽管这些术语的使用有时可能会重叠。[36]
只有30%到50%的概念在第一个三个月过去了。[37]绝大多数没有进步的人在女性意识到受孕之前就已经失去了[31],许多怀孕在医生检测到胚胎之前就已经失去了。[38]根据孕妇的年龄和健康状况,已知怀孕的15%至30%在临床明显流产期结束。[39]这些自然流产中有80%发生在孕早期。[40]
妊娠早期自然流产的最常见原因是胚胎或胎儿的染色体异常,[31] [41]占早期妊娠丢失量的至少50%。[42]其他原因包括血管疾病(如狼疮),糖尿病,其他激素问题,感染和子宫异常。[41]提高产妇年龄和女性先前自然流产的历史是导致自然流产风险增加的两个主要因素。[42]意外创伤也可引起自然流产;故意创伤或压力导致流产被认为是人工流产或堕胎。[43]
方法
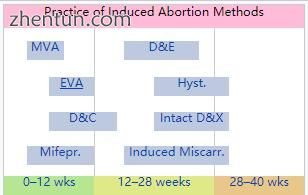
孕龄可以决定实施哪种堕胎方法。
药物
主要文章:药物流产
医疗堕胎是由堕胎药物诱发的堕胎。药物流产成为另一种流产方法,在20世纪70年代有前列腺素类似物和20世纪80年代抗孕激素米非司酮(也称为RU-486)。[5] [6] [44] [45] [46]
最常见的早期妊娠早期药物流产方案使用米非司酮联合前列腺素类似物(米索前列醇或前列素)至胎龄9周,甲氨蝶呤联合前列腺素类似物至多7周妊娠,或单独使用前列腺素类似物[ 44]米非司酮 - 米索前列醇联合用药比甲氨蝶呤 - 米索前列醇联合用药更快,在妊娠晚期更有效,联合用药比单用米索前列醇更有效。[45]该制度在妊娠中期有效。[47]在怀孕63天之前,在24至48小时之后,涉及米非司酮和米非司酮的药物流产团在面颊中有效。[48]
在早期流产,妊娠7周,使用米非司酮 - 米索前列醇联合方案的药物流产被认为比手术流产(真空吸引术)更有效,特别是当临床实践不包括对吸入组织的详细检查时。[49]使用米非司酮的早期药物流产方案,随后24-48小时后口服或阴道米索前列醇,在胎龄9周时有效率为98%。[50]如果药物流产失败,必须使用手术流产来完成手术。[51]
早期的医疗堕胎占英国孕前9周的大部分堕胎,[52] [53]法国,[54]瑞士,[55]和北欧国家。[56]在美国,截至2014年,早期医疗堕胎的比例约为30%。[57]
使用米非司酮联合前列腺素类似物的药物流产方案是加拿大,大多数欧洲,中国和印度使用的最常见的中期妊娠方法,[46]与美国相比,其中96%的孕中期流产率 通过扩张和疏散手术进行。[58]
外科
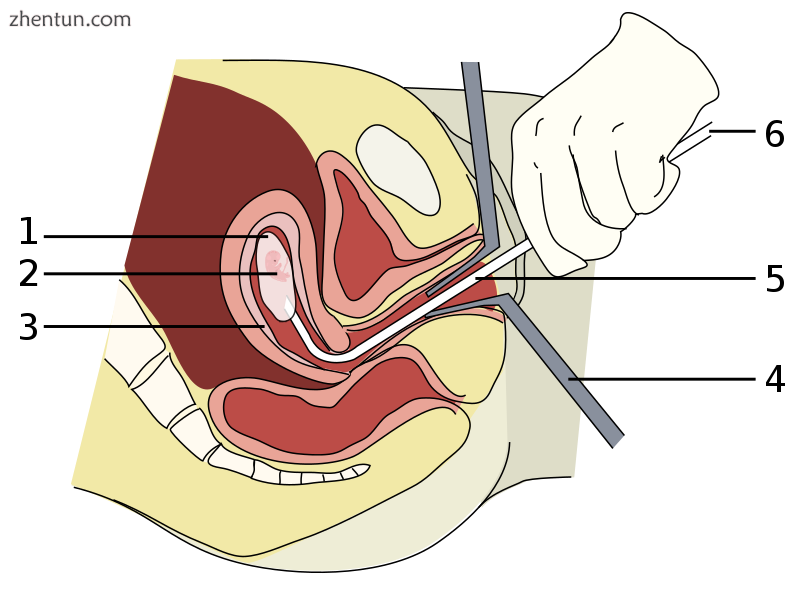
在孕周8周(受精后6周)进行真空吸引流产。
1:羊膜囊
2:胚胎
3:子宫内膜
4:窥器
5:Vacurette
6:安装在抽吸泵上
妊娠长达15周,吸痰或真空吸引是最常见的人工流产手术方法。[59]手动真空吸引术(MVA)包括使用手动注射器通过抽吸移除胎儿或胚胎,胎盘和膜,而电动真空抽吸(EVA)使用电动泵。这些技术的不同之处在于用于施加抽吸的机制,在怀孕早期如何使用,以及是否需要宫颈扩张。
MVA,也称为“微吸”和“月经提取”,可以在很早的怀孕期间使用,并且不需要宫颈扩张。扩张和刮宫术(D&C)是第二种最常见的手术流产方法,是一种标准的妇科手术,由于各种原因而进行,包括检查子宫内膜是否存在可能的恶性肿瘤,调查异常出血和流产。刮宫是指用刮匙清洁子宫壁。只有当MVA不可用时,世界卫生组织才推荐这种程序,也称为急性刮宫术。[60]
从妊娠第15周到大约26日,必须使用其他技术。扩张和撤离(D&E)包括打开子宫颈并使用手术器械和抽吸清空子宫颈。在妊娠第16周后,也可以通过完整的扩张和提取(IDX)(也称为宫内颅减压)诱导堕胎,这需要在撤离前对胎儿的头部进行手术减压。 IDX有时被称为“部分分娩流产”,在美国被联邦政府禁止。
在怀孕的第三个三个月,人工流产可以通过完整的扩张和拔除或通过子宫切开术手术进行。子宫切开术流产是一种类似于剖腹产的手术,在全身麻醉下进行。它需要比剖腹产更小的切口,并在怀孕的后期使用。[61]
妊娠早期手术通常可以使用局部麻醉进行,而孕中期方法可能需要深度镇静或全身麻醉。[62]
人工流产
在缺乏扩张和拔除所需的医疗技能的地方,或者从业者更喜欢的地方,可以通过先引诱分娩然后在必要时诱导胎儿死亡来诱导堕胎。[63]这有时被称为“诱导流产”。该过程可以从妊娠13周到妊娠晚期进行。虽然在美国非常罕见,但在整个孕中期超过80%的人工流产是瑞典和其他附近国家的人工流产。[64]
只有有限的数据可用于比较这种方法与扩张和提取。[64]与D&E不同,18周后的劳动力流产可能因胎儿短暂存活而复杂化,这可能在法律上被定性为活产。因此,在美国,劳动人工流产具有法律风险[64] [65]。
其他方法
历史上,许多据称具有堕胎特性的草药已被用于民间医学。其中包括:艾菊,薄荷属植物,黑升麻和现已灭绝的罗盘草。[66]:44-47,62-63,154-155,230-231
1978年,科罗拉多州的一名妇女在尝试通过服用薄荷油进行堕胎时死亡,另一名妇女严重受伤。[67]因为不加区分地使用草药作为堕胎药会导致严重甚至致命的副作用,例如多器官衰竭[68],医生不建议这样使用。
有时会通过对腹部造成创伤来尝试堕胎。如果严重的话,力度会导致严重的内伤,而不一定会成功引发流产。[69]在东南亚,有一种古老的传统,即通过强力腹部按摩来进行堕胎。[70]装饰柬埔寨吴哥窟的浮雕之一描绘了一名恶魔对一名被送往黑社会的妇女进行堕胎。[70]
报告的不安全自行流产方法包括误用米索前列醇,以及将非手术器具如针织衣架和衣架插入子宫内。这些和其他终止妊娠的方法可称为“诱导流产”。这些方法很少用于手术流产合法且可获得的国家。[71]
安全

南非的堕胎传单
堕胎的健康风险主要取决于该程序是安全还是不安全地进行。世界卫生组织将不安全堕胎定义为由非熟练人员,危险设备或不卫生设施进行的堕胎。[72]在发达国家进行的合法堕胎是最安全的医疗程序之一。[3] [73]在美国,堕胎造成的孕产妇死亡风险为每10万次手术造成的死亡风险为0.7,[4]堕胎妇女比分娩安全约13倍(每10万活产婴儿死亡人数为8.8)。[74] [75]在美国,从2000年到2009年,堕胎的死亡率低于整形手术。[76]与堕胎有关的死亡风险随着孕龄而增加,但至少在妊娠21周时仍然低于分娩的风险。[77] [78] [79]从妊娠64到70天,门诊流产安全有效,从57天到63天不等。[80]药物流产对于早于妊娠6周的妊娠是安全有效的。[81]
妊娠早期的真空吸引术是最安全的手术流产方法,可以在初级保健办公室,堕胎诊所或医院进行。罕见的并发症可能包括子宫穿孔,盆腔感染和需要第二次手术撤离的保留受孕产品。[82]感染占美国堕胎相关死亡人数的三分之一。[83]无论手术是在医院,手术中心还是办公室进行,妊娠早期真空吸引流产的并发症发生率相似。[84]预防性抗生素(如多西环素或甲硝唑)通常在选择性流产前给予,[85]因为它们被认为可以大大降低术后子宫感染的风险。[62] [86]根据堕胎是由医生还是中级医生执行,失败程序的比率似乎没有显着差异。[87]妊娠中期流产后的并发症与妊娠早期流产后的并发症相似,并且在某种程度上取决于所选择的方法。孕中期堕胎通常耐受良好。[88]
使用米非司酮联合米索前列醇和手术流产(真空抽吸)联合治疗妊娠早期妊娠9周的药物流产的安全性和有效性差异不大[49]。单独使用前列腺素类似物米索前列醇的药物流产比使用米非司酮和米索前列醇或手术流产的联合方案的药物流产效果更差且更痛苦。[89] [90]
一些据称堕胎的风险主要是由反堕胎组织推动的,[91] [92]但缺乏科学支持。[91]例如,已经广泛研究了人工流产与乳腺癌之间的联系问题。主要的医学和科学机构(包括世界卫生组织,国家癌症研究所,美国癌症协会,皇家OBGYN学院和美国国会OBGYN)得出的结论是,堕胎不会导致乳腺癌。[93]
在过去,甚至非法也不会自动意味着堕胎是不安全的。在谈到美国时,历史学家琳达戈登说:“事实上,这个国家的非法堕胎有着令人印象深刻的安全记录。”[94]:25根据Rickie Solinger的说法,
一个由广泛关注堕胎和公共政策的人发布的相关神话是,在合法化之前,堕胎者是肮脏而危险的后巷屠夫...... [9]他的历史证据并不支持这种说法。[95] :4
作者Jerome Bates和Edward Zawadzki描述了20世纪初美国东部非法堕胎者的案例,他为成功完成13,844次堕胎而感到自豪。[96]:59 1970年代纽约市着名的堕胎者/助产士Restell夫人(Anna Trow Lohman)似乎在超过100,000名患者中失去了极少数女性[97] - 死亡率低于当时的分娩死亡率。 1936年,着名的妇产科教授Frederick J. Taussig写道,在美国非法入狱期间,死亡率上升的原因是
随着过去五十年的每十年,这次事故[子宫穿孔]的实际和比例频率增加,首先是由于仪器诱导堕胎数量的增加;第二,医生处理的堕胎比例增加,而助产士处理的堕胎比例增加;第三,流行倾向于使用器械而不是手指来清空子宫。 [98]:223
精神健康
主要文章:堕胎和心理健康
目前的证据发现大多数人工流产与心理健康问题之间没有关系[8] [99],而不是任何意外怀孕的预期。[100]美国心理学会的一份报告得出的结论是,女性的第一次堕胎在头三个月进行时不会对精神健康构成威胁,这些女性不会比那些怀有意外怀孕的女性更容易出现心理健康问题。女性第二次或更大次堕胎的心理健康结果不太确定。[100] [101]一些较早的评论得出的结论是,堕胎与心理问题的风险增加有关; [102]但是,他们没有使用适当的对照组。[99]
虽然一些研究表明,由于胎儿异常,在孕早期选择堕胎的妇女的心理健康结果为负,[103]需要进行更严格的研究才能最终证明这一点。[104]一些被提议的堕胎的负面心理影响被反堕胎倡导者称为一种称为“堕胎后综合症”的单独病症,但美国的医学或心理专业人员并未认识到这一点。[105]
不安全的堕胎
主要文章:不安全堕胎

大约1925年的苏联海报,警告反对助产士进行堕胎。标题翻译:“由受过训练或自学成才的助产士进行的堕胎不仅会伤害女性,还会导致死亡。”
寻求终止妊娠的妇女有时采用不安全的方法,特别是在限制合法堕胎的情况下。他们可能会试图自我堕胎或依赖其他没有经过适当医疗培训或获得适当设施的人。这有导致严重并发症的趋势,例如不完全流产,败血症,出血和内脏损伤。[106]
不安全堕胎是全世界妇女受伤和死亡的主要原因。虽然数据不准确,但估计每年约有2000万次不安全堕胎,其中97%发生在发展中国家。[3]据信不安全堕胎会导致数百万人受伤。[3] [107]死亡人数估计数根据方法而有所不同,在过去十年中有37,000至70,000人不等; [3] [9] [108]不安全堕胎造成的死亡约占所有孕产妇死亡人数的13%。[109]世界卫生组织认为,自1990年代以来死亡率已下降。[110]为减少不安全堕胎的数量,公共卫生组织一般主张强调堕胎合法化,培训医务人员以及确保获得生殖健康服务。[111]作为回应,反对堕胎的人指出,堕胎禁令绝不会影响选择将胎儿带到足月的妇女的产前护理。 2012年签署的“关于孕产妇健康的都柏林宣言”指出,“禁止堕胎不会以任何方式影响孕妇获得最佳护理。”[112]
是否安全地进行堕胎的一个主要因素是堕胎的法律地位。与堕胎合法且可获得的堕胎相比,具有限制性堕胎法的国家的不安全堕胎率和类似的总体堕胎率相似。[9] [13] [111] [113] [114] [115] [116]例如,1996年南非堕胎合法化对堕胎相关并发症的频率产生了直接的积极影响,[117]与堕胎有关的死亡率下降了90%以上。[118]在其他国家放宽了堕胎法之后,例如罗马尼亚和尼泊尔,也观察到产妇死亡率的类似下降。[119] 2011年的一项研究得出结论,在美国,一些州级反堕胎法与该州较低的堕胎率相关。[120]然而,该分析没有考虑到没有这些堕胎法律的其他国家的旅行。[121]此外,缺乏有效避孕措施导致不安全堕胎。据估计,如果现代计划生育和产妇保健服务在全球范围内可以获得,不安全堕胎的发生率可降低多达75%(每年从2000万减少到500万)。[122]这种堕胎的比率可能难以衡量,因为它们可以被不同地报告为流产,“诱导流产”,“月经调节”,“小堕胎”和“延迟/暂停月经的调节”。[123] [124] ]
世界上40%的女性能够在妊娠期内接受治疗性和选择性堕胎[15],而另外35%的女性在符合某些身体,心理或社会经济标准的情况下可以进行合法堕胎。[17]虽然产妇死亡率很少是安全堕胎造成的,但不安全堕胎每年导致70,000人死亡和500万残疾。[9]不安全堕胎的并发症占全世界大约八分之一的孕产妇死亡,[125]尽管这种情况因地区而异。[126]不安全堕胎引起的继发性不孕影响了大约2400万妇女。[114] 1995年至2008年,不安全堕胎率从44%增加到49%。[13]为解决这一现象,已提出健康教育,获得计划生育以及改善堕胎期间和之后的医疗保健。[127]
活产
虽然这种情况非常罕见,但在妊娠18周后接受手术流产的妇女有时会生出可能短暂存活的胎儿。[128] [129] [130] 22周后可以长期存活。[131]
如果医务人员观察到生命迹象,他们可能需要提供护理:如果孩子有很好的生存机会,则需要紧急医疗护理;如果没有,则需要姑息治疗。[132] [133] [134]为避免这种情况,建议在妊娠20-21周后终止妊娠前诱导胎儿死亡。[135] [136] [137] [138] [139]
堕胎引起的活产死亡给出了ICD-10基本原因描述代码P96.4;数据被识别为胎儿或新生儿。在1999年至2013年期间,美国疾病预防控制中心记录了新生儿死亡人数531例,[140]每10万例堕胎中约有4例死亡。[141]
发生率
有两种常用的测量流产发生率的方法:
堕胎率 - 每1000名15至44岁妇女的堕胎数量
堕胎百分比 - 100例已知怀孕中的堕胎数量(怀孕包括活产,堕胎和流产)
在许多地方,堕胎是非法的或带有沉重的社会耻辱感,堕胎的医疗报告并不可靠。[113]因此,必须在不确定与标准误差相关的确定性的情况下估算堕胎的发生率。[13]
近年来,全世界的堕胎数量似乎保持稳定,2003年有4160万人,2008年有4380万人。[13]全世界的堕胎率为每千名妇女28人,但发达国家为每千名妇女24人,发展中国家为每1000名妇女29人。[13]同一项2012年的研究表明,2008年,全世界已知怀孕的估计堕胎率为21%,发达国家为26%,发展中国家为20%。[13]
平均而言,堕胎的发生率在具有限制性堕胎法的国家和更容易获得堕胎的国家中是相似的。但是,限制性堕胎法与不安全堕胎百分比的增加有关。[15] [142] [143]发展中国家不安全的堕胎率部分归因于无法获得现代避孕药具;据古特马赫研究所称,提供避孕药具将使全世界每年不安全堕胎减少约1450万人,减少38,000人死于不安全堕胎。[144]
法律,人工流产率在世界范围内差异很大。根据Guttmacher研究所员工的报告,2008年在统计数据完全统计的国家中,每1000名妇女(德国和瑞士)为7名,每1000名妇女(爱沙尼亚)为30名。人工流产结束的怀孕比例约为10 %(以色列,荷兰和瑞士)占同一组别的30%(爱沙尼亚),但在匈牙利和罗马尼亚可能高达36%,其统计数据被认为是不完整的。[145] [146]
堕胎率也可以表示为妇女在生育年龄期间的平均堕胎数量;这被称为总堕胎率(TAR)。
孕龄和方法
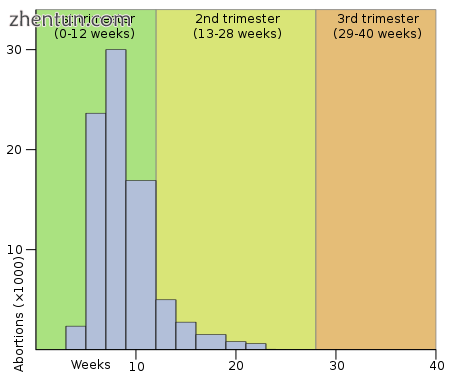
2004年英格兰和威尔士孕龄堕胎直方图。(左)
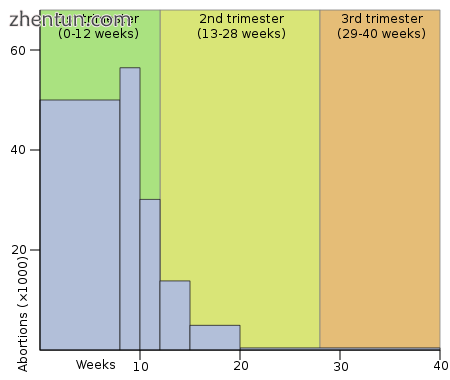
2004年孕龄在美国的堕胎。(右)
堕胎率也取决于怀孕阶段和实践方法。 2003年,美国疾病控制和预防中心(CDC)报告称,据报道,美国报告的合法人工流产率为26%,孕期不到6周,7周时为18%,8岁时为15%。周,9至10周时为18%,11至12周时为9.7%,13至15周时为6.2%,16至20周时为4.1%,超过21周时为1.4%。其中90.9%被分类为“刮宫术”(吸痰,扩张和刮宫,扩张和撤离),7.7%用“医疗”方式(米非司酮),0.4%用“宫内滴注”(盐水或前列腺素) )和“其他”(包括子宫切开术和子宫切除术)的1.0%。[147]根据疾病预防控制中心的说法,由于数据收集困难,数据必须被视为暂定的,如果通过与人工流产相同的程序完成死胎的移除,则报告超过20周的一些胎儿死亡可能是自然死亡被错误地归类为堕胎。[148]
Guttmacher研究所估计,2000年美国有2,200个完整的扩张和提取程序;这占当年堕胎总数的0.17%。[149]同样,在2006年的英格兰和威尔士,89%的终止发生在12周或12周以下,9%发生在13周和19周之间,1.5%发生在20周或20周以上。报告的64%是真空抽吸,6%是D&E,30%是医疗。[150]中国,印度和越南等发展中国家的孕中期堕胎数量超过发达国家。[151]
动机
个人
妇女堕胎的原因多种多样,而且在世界各地都有所不同。[148] [152]
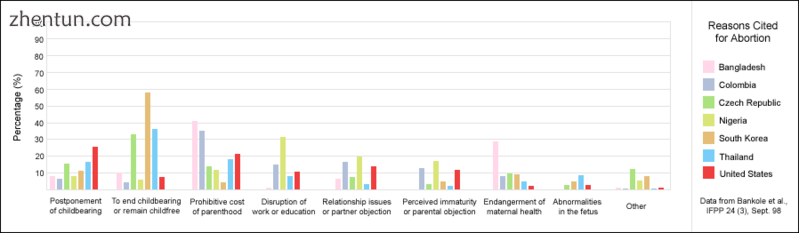
一张条形图,描绘了一份1998年AGI元研究中的选定数据,该研究报告了妇女堕胎的原因。
一些最常见的原因是将生育推迟到更合适的时间或将精力和资源集中在现有儿童身上。其他包括无论是抚养孩子的直接成本还是在照顾孩子时失去收入,父亲缺乏支持,无力支付额外的孩子,为现有儿童提供教育的愿望,都无法负担孩子的费用。 ,破坏自己的教育,与伴侣的关系问题,过于年幼,不能生孩子,失业,以及不愿意抚养因强奸或乱伦等原因而被抚养的孩子。[152] [ 153]
社会
由于社会压力,一些堕胎经历了。这些可能包括偏爱特定性别或种族的儿童,[154]不赞成单身或早期母亲,对残疾人的侮辱,对家庭的经济支持不足,无法获得或拒绝避孕方法,或对人口的努力控制(如中国的独生子女政策)。这些因素有时会导致强制堕胎或性别选择性堕胎。[155] [未引用]
2002年的一项美国研究得出结论,大约一半的堕胎妇女在怀孕时使用了一种避孕方法。一半使用安全套的人和使用避孕药的人中有四分之一报告使用不一致;使用安全套的人中有42%报告因滑倒或破损而失败。[156]古特马赫研究所估计,“美国大多数堕胎都是少数民族妇女”,因为少数民族妇女“意外怀孕率高得多”。[157]
孕产妇和胎儿的健康
另一个因素是孕产妇或胎儿健康的风险,这被认为是一些国家超过三分之一的堕胎的主要原因,并且是其他国家仅有一位数百分比的堕胎的重要因素。[148] [152]
在美国,最高法院在Roe v.Wade和Doe诉Bolton案中的判决:“裁定国家对胎儿生命的兴趣仅在生存能力方面变得引人注目,定义为胎儿可以存活的点独立于母亲。即使在生存能力之后,国家也不能支持胎儿的生命对孕妇的生命或健康的影响。在隐私权下,医生必须自由地使用他们的“医学判断来保护母亲的生命或健康状况。“在法院判决Roe的同一天,它还决定了Doe诉Bolton,其中法院对健康的定义非常广泛:”医疗判决可以根据所有因素行使 - 身体,情感,心理,家庭和女性的年龄 - 与患者的福祉相关。所有这些因素都可能与健康有关。这使得主治医生能够做出最佳医学判断所需的空间。“[158]:1200-1201
在电视名人Sherri Finkbine在怀孕第五个月发现她接触过沙利度胺之后,公众舆论在美国转移。由于无法在美国获得合法堕胎,她前往瑞典。从1962年到1965年,德国麻疹爆发导致15,000名婴儿出现严重的先天缺陷。 1967年,美国医学会公开支持堕胎法的自由化。 1965年的一项全国舆论研究中心民意调查显示,当母亲的生命处于危险之中时,73%支持堕胎,出生缺陷时为57%,强奸或乱伦导致妊娠占59%。[159]
癌症
怀孕期间的癌症发病率为0.02-1%,并且在许多情况下,母亲的癌症导致考虑流产以保护母亲的生命,或者响应于治疗期间胎儿可能发生的潜在损害。对于宫颈癌尤其如此,其中最常见的类型发生在每2,000-13,000例妊娠中的1例中,其中治疗的开始“不能与保持胎儿生命共存(除非选择新辅助化疗)”。非常早期的宫颈癌(I和IIa)可以通过根治性子宫切除术和盆腔淋巴结清扫术,放射疗法或两者来治疗,而后期阶段通过放射治疗来治疗。化疗可以同时使用。怀孕期间治疗乳腺癌也涉及胎儿因素,因为不鼓励乳房肿瘤切除术有利于改良根治性乳房切除术,除非晚期妊娠允许在分娩后进行随访放射治疗。[160]
接触单一化疗药物估计会对胎儿造成7.5-17%的致畸作用风险,多种药物治疗的风险更高。超过40 Gy的辐射治疗通常会导致自然流产。在妊娠早期,特别是8至15周的发育期间接触低得多的剂量可导致智力残疾或小头畸形,并且在此阶段或后续阶段的暴露可导致胎儿宫内发育和出生体重减少。暴露于0.005-0.025 Gy之间会导致智商的剂量依赖性降低[160]。根据被照射的区域离胎儿的距离,可以大大减少腹部屏蔽对辐射的影响。[161] [162]
出生过程本身也可能使母亲处于危险之中。 “阴道分娩可能导致肿瘤细胞扩散到淋巴血管通道,出血,宫颈裂伤和外阴切开术部位的恶性细胞植入,而腹部分娩可能会延迟非手术治疗的开始。”[163]
历史和宗教
主要文章:堕胎史

在柬埔寨吴哥窟的浅浮雕,c. 1150年,描绘了一个通过用杵敲打孕妇腹部诱导堕胎的恶魔。[70] [164]
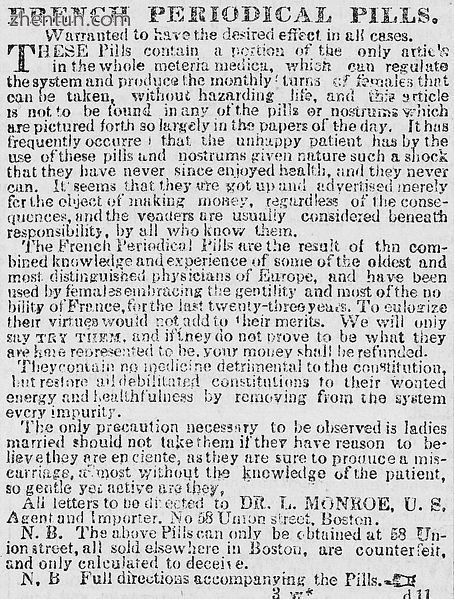
“法国期刊丸”。 1845年1月出版的“波士顿每日时报”刊登的秘密广告的一个例子。
自古以来,人们就已经使用草药,尖锐的工具,用武力或通过其他传统方法进行堕胎。[16]人工流产历史悠久,可以追溯到神农(公元前2700年左右),古埃及及其埃伯斯纸莎草(公元前1550年),以及青年时期罗马帝国(c)的文明。 .200 CE)。[16]有证据表明怀孕是通过多种方法终止的,包括堕胎药物的使用,尖锐器具的使用,腹压的应用以及其他技术。最早已知的堕胎艺术表现形式之一是吴哥窟的浅浮雕(约1150年)。在印度教和佛教文化中代表死后判断的一系列饰带中,它描绘了腹部流产的技术。[70]
一些医学学者和堕胎反对者认为希波克拉底誓言禁止古希腊医生进行堕胎; [16]其他学者不同意这种解释,[16]并指出希波克拉底语语料库的医学文本包含对堕胎技术的描述。宣誓。[165]医生Scribonius Largus在公元43年写道,希波克拉底誓言禁止堕胎,Soranus也是如此,尽管当时并非所有医生都严格遵守堕胎。根据Soranus的第一或第二世纪CE工作妇科学,一个医疗从业者党按照希波克拉底誓言的要求消灭了所有堕胎;另一方 - 他所属的 - 愿意开堕胎,但只是为了母亲的健康。[166] [167]
亚里士多德在他关于政治政治的论文(公元前350年)中,谴责杀婴是一种人口控制手段。在这种情况下,他更倾向于堕胎,并且限制[168]“必须在它产生感觉和生命之前对其实施;因为合法和非法堕胎之间的界限将以感觉和存在的事实为标志。活着。” [169]在基督教中,教皇西斯图斯五世(1585-90)是1869年之前唯一一位宣布堕胎是凶杀的教皇,无论怀孕阶段如何; [170]他的继承人在三年后宣布他的1588年宣告被撤销。在其历史的大部分时间里,天主教会对是否认为堕胎是谋杀是否存在分歧,并且直到19世纪才开始大力反对堕胎。[16]事实上,一些历史学家写过[171] [172] [173],在19世纪之前,大多数天主教作者并未将“加速”或“堕胎”作为堕胎之前终止妊娠。
1995年的一项调查报告说,天主教女性与一般人群一样可以终止妊娠,新教徒不太可能这样做,而福音派基督徒最不可能这样做。[148] [152]传统上,伊斯兰传统允许堕胎,直到穆斯林相信灵魂进入胎儿的时间点,[16]各种神学家认为受孕,受孕后40天,受孕后120天或加速。[174]但是,在伊斯兰教信仰高的地区,如中东和北非,堕胎受到严重限制或禁止。[175]
在欧洲和北美,堕胎技术从17世纪开始发展。然而,大多数医生对性问题的保守性阻碍了安全堕胎技术的广泛扩展。[16]除了一些医生之外,其他医生也在宣传他们的服务,直到19世纪才开始对他们进行广泛监管,当时美国和英国都禁止这种做法(有时称为restellism)[176]。[16]教会团体和医生在反堕胎运动中具有很大的影响力。[16]在美国,根据一些消息来源,堕胎比分娩更危险,直到大约1930年,堕胎手术相对于分娩的逐步改善使堕胎更安全。[注2]然而,其他消息来源认为,在19世纪卫生的早期堕胎助产士通常工作的条件相对安全。[177] [178] [179]此外,一些评论员写道,尽管医疗程序有所改善,但从20世纪30年代到合法化期间,反堕胎法律的执行也更加热烈,同时有组织犯罪对堕胎服务提供者的控制也越来越多。[180] [181] [182] [183]​​ [184]
苏联俄罗斯(1919年),冰岛(1935年)和瑞典(1938年)是最早将某些或所有形式的堕胎合法化的国家之一。[185] 1935年,纳粹德国通过了一项法律,允许对那些被视为“遗传性疾病”的人进行堕胎,而被认为是德国种群的妇女则被明确禁止堕胎。[186]从二十世纪下半叶开始,堕胎在更多的国家合法化。[16]
社会与文化
堕胎辩论
主要文章:堕胎辩论
人工流产一直是引起大量争论的根源。围绕堕胎的道德,道德,哲学,生物,宗教和法律问题与价值体系有关。关于堕胎的意见可能涉及胎儿权利,政府权威和妇女权利。
在公开辩论和私人辩论中,赞成或反对堕胎获取的论点集中于人工流产的道德允许性,或者允许或限制堕胎的法律的理由。[187]世界医学会关于治疗性堕胎的宣言指出,“使母亲的利益与其未出生的孩子的利益发生冲突的情况造成了两难,并提出了是否应故意终止怀孕的问题。”[188]堕胎辩论,特别是与堕胎法有关的堕胎辩论,往往由倡导这两个职位之一的团体牵头。支持对堕胎采取更多法律限制的反堕胎团体,包括完全禁止,往往称自己为“依赖生命”,而反对这种法律限制的堕胎权利团体则称自己为“支持选择”。[189]一般来说,前者的立场认为,人类胎儿是一个有生命权的人,使堕胎在道德上与谋杀一样。后一种观点认为,妇女具有一定的生殖权利,特别是决定是否怀孕的权利。
现代流产法
主要文章:堕胎法
另见:堕胎法辩论的历史
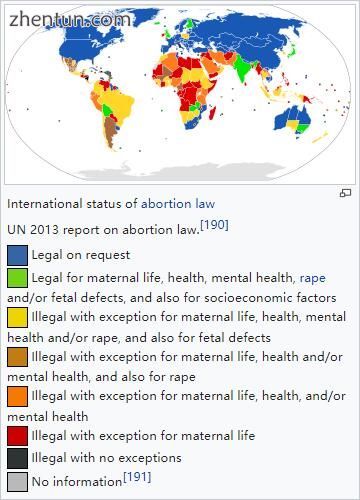
堕胎法的国际地位
联合国2013年关于堕胎法的报告。[190]
  法律要求
  对产妇生命,健康,心理健康,强奸和/或胎儿缺陷以及社会经济因素的法律保护
  对于孕产妇,健康,精神健康和/或强奸以及胎儿缺陷都是非法的
  对于孕产妇,健康和/或心理健康以及强奸都是非法的
  非生育,健康和/或心理健康的例外情况
  非产妇生活例外
  非法,没有例外
  没有资料[191]
目前有关堕胎的法律是多种多样的。宗教,道德和文化因素继续影响着全世界的堕胎法。生命权,自由权,人身安全权和生殖健康权是人权的主要问题,有时构成堕胎法存在或不存在的基础。
在堕胎合法的司法管辖区,在妇女获得安全合法堕胎之前必须经常满足某些要求(未经妇女同意而进行的堕胎被视为堕胎)。这些要求通常取决于胎儿的年龄,通常使用基于三个月的系统来调节合法性的窗口,或者像美国一样,根据医生对胎儿活力的评估。有些司法管辖区要求在程序前等待一段时间,规定有关胎儿发育的资料分布,或要求在未成年女儿要求堕胎时与父母联络。[192]其他司法管辖区可能要求妇女在中止胎儿之前获得胎儿父亲的同意,堕胎提供者告知妇女该程序的健康风险 - 有时包括医学文献不支持的“风险” - 并且多个医疗机构认证堕胎在医学上或社会上是必要的。在紧急情况下可以免除许多限制。中国已经结束了[193]独生子女政策,现在有了两个孩子的政策,[194] [195]有时将强制堕胎作为其人口控制战略的一部分。[196]
其他司法管辖区几乎完全禁止堕胎。许多(但不是全部)允许在各种情况下进行合法堕胎。这些情况因管辖权而异,但可能包括怀孕是由于强奸还是乱伦,胎儿的发育受损,妇女的身心健康受到威胁,还是社会经济因素导致分娩困难。[17]在完全禁止堕胎的国家,如尼加拉瓜,医疗当局因怀孕而直接和间接地导致孕产妇死亡率上升,以及由于医生担心如果他们治疗其他妇科紧急情况而可能会因死亡而死亡。[197] [198]一些国家,如孟加拉国,名义上禁止堕胎,也可能支持以月经卫生为幌子进行堕胎的诊所。[199]这也是传统医学的术语。[200]在堕胎非法或带有严重社会耻辱感的地方,孕妇可以从事医疗旅游并前往可以终止妊娠的国家。[201]没有旅行手段的妇女可以诉诸非法堕胎提供者或试图自行堕胎。[202]
自1999年以来,女性波浪组织一直在提供有关医疗堕胎的教育。该非政府组织在一个集装箱内创建了一个移动医疗诊所,然后在租用的船上前往具有限制性堕胎法的国家。由于船舶在荷兰注册,因此当船舶在国际水域时,荷兰法律占主导地位。在港口,该组织提供免费的讲习班和教育;在国际水域,医务人员在法律上能够开出药物流产药物和咨询。[203] [204] [205]
性别选择性流产
主要文章:性别选择性流产
超声和羊膜穿刺术允许父母在分娩前确定性别。这项技术的发展导致性别选择性堕胎,或基于性别终止胎儿。选择性终止女性胎儿是最常见的。
性别选择性堕胎是造成一些国家男女儿童出生率明显不同的部分原因。据报道,亚洲许多地区都存在对男孩的偏好,台湾,韩国,印度和中国报告了用于限制女性出生的堕胎。[206]尽管有关国家可能已正式禁止性别选择性堕胎甚至性别筛查,但这种情况与男性和女性的标准出生率有所偏差。[207] [208] [209] [210]在中国,1979年颁布的独生子女政策加剧了对男童的历史偏好。[211]
许多国家已采取立法措施,以减少性别选择性堕胎的发生率。在1994年国际人口与发展会议上,180多个国家同意消除“对女童的一切形式歧视和儿子偏好的根本原因”,[212]条件也在2011年的PACE决议中受到谴责。[213]世界卫生组织和联合国儿童基金会以及联合国其他机构发现,减少性堕胎的措施在减少性别选择性堕胎方面的效果远远低于减少性别不平等的措施。[212]
反堕胎暴力
主要文章:反堕胎暴力
在许多情况下,堕胎提供者和这些设施遭受各种形式的暴力,包括谋杀,谋杀未遂,绑架,跟踪,殴打,纵火和爆炸。政府和学术界将反堕胎暴力列为恐怖主义。[214] [215]只有一小部分反对堕胎的人实施暴力。
在美国,四名进行堕胎的医生被谋杀:David Gunn(1993),John Britton(1994),Barnett Slepian(1998)和George Tiller(2009)。在美国和澳大利亚,还有其他人员在堕胎诊所就诊,其中包括接待员和保安人员,如詹姆斯巴雷特,香农洛尼,李安尼科尔斯和罗伯特桑德森。伤口(例如,Garson Romalis)和谋杀未遂也发生在美国和加拿大。发生了数百次爆炸,纵火,酸性袭击,入侵以及对堕胎提供者的破坏事件。[216] [217]着名的反堕胎暴力犯罪者包括Eric Robert Rudolph,Scott Roeder,Shelley Shannon和Paul Jennings Hill,他们是第一个因谋杀堕胎提供者而在美国被处决的人。[218]
在堕胎合法的一些国家,已经对堕胎获得法律保护。这些法律通常旨在保护堕胎诊所免受阻挠,故意破坏,纠察和其他行为的侵害,或保护这些设施的妇女和雇员免受威胁和骚扰。
比身体暴力更常见的是心理压力。 2003年,克里斯丹泽在德克萨斯州组织了支持生命的组织,以防止在奥斯汀建立计划生育设施。这些组织在网上发布了个人信息,涉及建设者,每天最多发送1200个电话并联系他们的教堂。[219]一些抗议者记录妇女在相机上进入诊所。[219]
其他动物
更多信息:流产
各种动物都会发生自然流产。例如,在绵羊中,它可能是由压力或体力消耗引起的,例如通过门挤或被狗追逐。[220]在奶牛中,流产可能是由传染性疾病引起的,例如布鲁氏菌病或弯曲杆菌,但通常可以通过接种疫苗来控制。[221]吃松针还可以诱导奶牛堕胎。[222] [223]已知有几种植物,包括苦菜,臭鼬卷心菜,毒铁杉和树烟,会导致牛的胎儿畸形和流产[224]:45-46以及绵羊和山羊。[224]:77-80在马,a如果胎儿有致命的白色综合征(先天性肠神经节病),胎儿可能会被流产或再吸收。对于显性白色基因(WW)纯合的驹胚胎理论上也在出生前被中止或再吸收。[225]在许多种类的鲨鱼和rays鱼中,在捕获时经常发生应激性流产。[226]
病毒感染可导致狗流产。[227]由于多种原因,猫可能会经历自然流产,包括荷尔蒙不平衡。对怀孕的猫进行联合堕胎和喷洒,特别是在Trap-Neuter-Return计划中,以防止不想要的小猫出生。[228] [229] [230]当雌性啮齿动物暴露于不负责怀孕的男性的气味时,可以终止怀孕,称为布鲁斯效应。[231]
在畜牧业的背景下,也可以在动物中诱导流产。例如,堕胎可能是在母马中引起的,这些母马交配不当,或者是那些没有意识到母马怀孕或怀有双胞胎马驹的主人购买的。[232]由于男性对母马的骚扰或强迫交配,马匹和斑马可能会发生杀戮,[233] [234] [235]尽管野外频率受到质疑。[236]雄性灰叶猴可能会在男性接管后攻击雌性,导致流产。[237]
说明:
Definitions of abortion, as with many words, vary from source to source. Language used to define abortion often reflects societal and political opinions (not only scientific knowledge). For a list of definitions as stated by obstetrics and gynecology (OB/GYN) textbooks, dictionaries, and other sources, please see Definitions of abortion.
By 1930, medical procedures in the US had improved for both childbirth and abortion but not equally, and induced abortion in the first trimester had become safer than childbirth. In 1973, Roe v. Wade acknowledged that abortion in the first trimester was safer than childbirth:
"The 1970s". Time communication 1940–1989: retrospective. Time Inc. 1989. Blackmun was also swayed by the fact that most abortion prohibitions were enacted in the 19th century when the procedure was more dangerous than now.
Will, George (1990). Suddenly: the American idea abroad and at home, 1986–1990. Free Press. p. 312. ISBN 0-02-934435-2.
Lewis, J.; Shimabukuro, Jon O. (28 January 2001). "Abortion Law Development: A Brief Overview". Congressional Research Service. Archived from the original on 14 May 2011. Retrieved 1 May 2011.
*Schultz, David Andrew (2002). Encyclopedia of American law. Infobase Publishing. p. 1. ISBN 0-8160-4329-9. Archived from the original on 9 December 2015.
Lahey, Joanna N. (24 September 2009). "Birthing a Nation: Fertility Control Access and the 19th Century Demographic Transition" (PDF; preliminary version). Colloquium. Pomona College. Archived (PDF) from the original on 7 January 2012.
参考
"Abortion (noun)". Oxford Living Dictionaries. Retrieved 8 June 2018. [mass noun] The deliberate termination of a human pregnancy, most often performed during the first 28 weeks of pregnancy
Grimes, DA; Stuart, G (2010). "Abortion jabberwocky: the need for better terminology". Contraception. 81 (2): 93–6. doi:10.1016/j.contraception.2009.09.005. PMID 20103443.
Grimes, DA; Benson, J; Singh, S; Romero, M; Ganatra, B; Okonofua, FE; Shah, IH (2006). "Unsafe abortion: The preventable pandemic" (PDF). The Lancet. 368 (9550): 1908–1919. doi:10.1016/S0140-6736(06)69481-6. PMID 17126724. Archived (PDF) from the original on 29 June 2011.
Raymond, EG; Grossman, D; Weaver, MA; Toti, S; Winikoff, B (November 2014). "Mortality of induced abortion, other outpatient surgical procedures and common activities in the United States". Contraception. 90 (5): 476–479. doi:10.1016/j.contraception.2014.07.012. PMID 25152259.
Kulier, R; Kapp, N; Gülmezoglu, AM; Hofmeyr, GJ; Cheng, L; Campana, A (9 November 2011). "Medical methods for first trimester abortion". The Cochrane Database of Systematic Reviews (11): CD002855. doi:10.1002/14651858.CD002855.pub4. PMID 22071804.
Kapp, N; Whyte, P; Tang, J; Jackson, E; Brahmi, D (September 2013). "A review of evidence for safe abortion care". Contraception. 88 (3): 350–63. doi:10.1016/j.contraception.2012.10.027. PMID 23261233.
"Abortion - Women's Health Issues". Merck Manuals Consumer Version. Retrieved 12 July 2018.
Lohr, PA; Fjerstad, M; Desilva, U; Lyus, R (2014). "Abortion". BMJ. 348: f7553. doi:10.1136/bmj.f7553.
Shah, I; Ahman, E (December 2009). "Unsafe abortion: global and regional incidence, trends, consequences, and challenges" (PDF). Journal of Obstetrics and Gynaecology Canada. 31 (12): 1149–58. doi:10.1016/s1701-2163(16)34376-6. PMID 20085681. Archived from the original (PDF) on 16 July 2011.
World Health Organization (2012). Safe abortion: technical and policy guidance for health systems (PDF) (2nd ed.). Geneva: World Health Organization. p. 8. ISBN 9789241548434. Archived (PDF) from the original on 16 January 2015.
Sedgh, Gilda; Bearak, Jonathan; Singh, Susheela; Bankole, Akinrinola; Popinchalk, Anna; Ganatra, Bela; Rossier, Clémentine; Gerdts, Caitlin; Tunçalp, Özge; Johnson, Brooke Ronald; Johnston, Heidi Bart; Alkema, Leontine (May 2016). "Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends". The Lancet. 388: 258–67. doi:10.1016/S0140-6736(16)30380-4. PMC 5498988. PMID 27179755.
"Worldwide, an estimated 25 million unsafe abortions occur each year". World Health Organization. 28 September 2017. Retrieved 29 September 2017.
Sedgh, G.; Singh, S.; Shah, I. H.; Åhman, E.; Henshaw, S. K.; Bankole, A. (2012). "Induced abortion: Incidence and trends worldwide from 1995 to 2008" (PDF). The Lancet. 379 (9816): 625–632. doi:10.1016/S0140-6736(11)61786-8. PMID 22264435. Archived (PDF) from the original on 6 February 2012. Because few of the abortion estimates were based on studies of random samples of women, and because we did not use a model-based approach to estimate abortion incidence, it was not possible to compute confidence intervals based on standard errors around the estimates. Drawing on the information available on the accuracy and precision of abortion estimates that were used to develop the subregional, regional, and worldwide rates, we computed intervals of certainty around these rates (webappendix). We computed wider intervals for unsafe abortion rates than for safe abortion rates. The basis for these intervals included published and unpublished assessments of abortion reporting in countries with liberal laws, recently published studies of national unsafe abortion, and high and low estimates of the numbers of unsafe abortion developed by WHO.
Sedgh G, Henshaw SK, Singh S, Bankole A, Drescher J (September 2007). "Legal abortion worldwide: incidence and recent trends". International Family Planning Perspectives. 33 (3): 106–116. doi:10.1363/ifpp.33.106.07. PMID 17938093. Archived from the original on 19 August 2009.
Culwell KR, Vekemans M, de Silva U, Hurwitz M (July 2010). "Critical gaps in universal access to reproductive health: Contraception and prevention of unsafe abortion". International Journal of Gynecology & Obstetrics. 110: S13–16. doi:10.1016/j.ijgo.2010.04.003. PMID 20451196.
Paul, M; Lichtenberg, ES; Borgatta, L; Grimes, DA; Stubblefield, PG; Creinin, MD; Joffe, Carole (2009). "1. Abortion and medicine: A sociopolitical history". Management of Unintended and Abnormal Pregnancy (PDF) (1st ed.). Oxford, United Kingdom: John Wiley & Sons, Ltd. ISBN 978-1-4443-1293-5. OL 15895486W. Archived (PDF) from the original on 21 October 2011.
Boland, R.; Katzive, L. (2008). "Developments in Laws on Induced Abortion: 1998–2007". International Family Planning Perspectives. 34 (3): 110–120. doi:10.1363/ifpp.34.110.08. PMID 18957353. Archived from the original on 7 October 2011.
Paola, Adolf; Walker, Robert; LaCivita, Lois (2010). Nixon, Frederick, ed. Medical ethics and humanities. Sudbury, Mass.: Jones and Bartlett Publishers. p. 249. ISBN 9780763760632. OL 13764930W. Archived from the original on 6 September 2017.
Johnstone, Megan-Jane (2009). Bioethics a nursing perspective (5th ed.). Sydney, N.S.W.: Churchill Livingstone/Elsevier. p. 228. ISBN 9780729578738. Archived from the original on 6 September 2017. Although abortion has been legal in many countries for several decades now, its moral permissibilities continues to be the subject of heated public debate.
Pastor Mark Driscoll (18 October 2013). "What do 55 million people have in common?". Fox News. Archived from the original on 31 August 2014. Retrieved 2 July 2014.
Hansen, Dale (18 March 2014). "Abortion: Murder, or Medical Procedure?". The Huffington Post. Archived from the original on 14 July 2014. Retrieved 2 July 2014.
Sifris, Ronli Noa (2013). Reproductive freedom, torture and international human rights: challenging the masculinisation of torture. Hoboken: Taylor & Francis. p. 3. ISBN 9781135115227. OCLC 869373168. Archived from the original on 15 October 2015.
Swett, C. (2007). Unsafe abortion : global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003 (5th ed.). World Health Organization. ISBN 9789241596121.
"Abortion - medical". US National Library of Medicine (Medline Plus). 9 July 2018.
Cheng L. (1 November 2008). "Surgical versus medical methods for second-trimester induced abortion". The WHO Reproductive Health Library. World Health Organization. Archived from the original on 17 June 2011. Retrieved 17 June 2011.
Bankole; et al. (1998). "Reasons Why Women Have Induced Abortions: Evidence from 27 Countries". International Family Planning Perspectives. 24 (3): 117–127 & 152. doi:10.2307/3038208. Archived from the original on 17 January 2006.
Finer, Lawrence B.; Frohwirth, Lori F.; Dauphinee, Lindsay A.; Singh, Susheela; Moore, Ann M. (2005). "Reasons U.S. Women Have Abortions: Quantitative and Qualitative Perspectives" (PDF). Perspectives on Sexual and Reproductive Health. 37 (3): 110–118. doi:10.1111/j.1931-2393.2005.tb00045.x. PMID 16150658. Archived (PDF) from the original on 17 January 2006.
Stubblefield, Phillip G. (2002). "10. Family Planning". In Berek, Jonathan S. Novak's Gynecology (13 ed.). Lippincott Williams & Wilkins. ISBN 978-0-7817-3262-8.
Bartlett, LA; Berg, CJ; Shulman, HB; Zane, SB; Green, CA; Whitehead, S; Atrash, HK (2004), "Risk factors for legal induced abortion-related mortality in the United States", Obstetrics & Gynecology, 103 (4): 729–37, doi:10.1097/01.AOG.0000116260.81570.60, PMID 15051566
Roche, Natalie E. (28 September 2004). "Therapeutic Abortion". eMedicine. Archived from the original on 14 December 2004. Retrieved 19 June 2011.
Schorge, John O.; Schaffer, Joseph I.; Halvorson, Lisa M.; Hoffman, Barbara L.; Bradshaw, Karen D.; Cunningham, F. Gary, eds. (2008). "6. First-Trimester Abortion". Williams Gynecology (1 ed.). McGraw-Hill Medical. ISBN 978-0-07-147257-9.
"Elective surgery". Encyclopedia of Surgery. Archived from the original on 13 November 2012. Retrieved 17 December 2012. "An elective surgery is a planned, non-emergency surgical procedure. It may be either medically required (e.g., cataract surgery), or optional (e.g., breast augmentation or implant) surgery.
Churchill Livingstone medical dictionary. Edinburgh New York: Churchill Livingstone Elsevier. 2008. ISBN 978-0-443-10412-1. The preferred term for unintentional loss of the product of conception prior to 24 weeks' gestation is miscarriage.
Annas, George J.; Elias, Sherman (2007). "51. Legal and Ethical Issues in Obstetric Practice". In Gabbe, Steven G.; Niebyl, Jennifer R.; Simpson, Joe Leigh. Obstetrics: Normal and Problem Pregnancies (5 ed.). Churchill Livingstone. p. 669. ISBN 978-0-443-06930-7. A preterm birth is defined as one that occurs before the completion of 37 menstrual weeks of gestation, regardless of birth weight.
"Stillbirth". Concise Medical Dictionary. Oxford University Press. 2010. Archived from the original on 15 October 2015. birth of a fetus that shows no evidence of life (heartbeat, respiration, or independent movement) at any time later than 24 weeks after conception
"7 FAM 1470 Documenting Stillbirth (Fetal Death)". United States Department of State. 18 February 2011. Retrieved 12 January 2016.
Annas, George J.; Elias, Sherman (2007). "24. Pregnancy loss". In Gabbe, Steven G.; Niebyl, Jennifer R.; Simpson, Joe Leigh. Obstetrics: Normal and Problem Pregnancies (5 ed.). Churchill Livingstone. ISBN 978-0-443-06930-7.
Katz, Vern L. (2007). "16. Spontaneous and Recurrent Abortion – Etiology, Diagnosis, Treatment". In Katz, Vern L.; Lentz, Gretchen M.; Lobo, Rogerio A.; Gershenson, David M. Katz: Comprehensive Gynecology (5 ed.). Mosby. ISBN 978-0-323-02951-3.
Stovall, Thomas G. (2002). "17. Early Pregnancy Loss and Ectopic Pregnancy". In Berek, Jonathan S. Novak's Gynecology (13 ed.). Lippincott Williams & Wilkins. ISBN 978-0-7817-3262-8.
Cunningham, F. Gary; Leveno, Kenneth J.; Bloom, Steven L.; Spong, Catherine Y.; Dashe, Jodi S.; Hoffman, Barbara L.; Casey, Brian M.; Sheffield, Jeanne S., eds. (2014). Williams Obstetrics (24th ed.). McGraw Hill Education. ISBN 978-0-07-179893-8.
Stöppler, Melissa Conrad. Shiel, William C., Jr., ed. "Miscarriage (Spontaneous Abortion)". MedicineNet.com. WebMD. Archived from the original on 29 August 2004. Retrieved 7 April 2009.
Jauniaux E, Kaminopetros P, El-Rafaey H (1999). "Early pregnancy loss". In Whittle MJ, Rodeck CH. Fetal medicine: basic science and clinical practice. Edinburgh: Churchill Livingstone. p. 837. ISBN 978-0-443-05357-3. OCLC 42792567.
"Fetal Homicide Laws". National Conference of State Legislatures. Archived from the original on September 11, 2012. Retrieved 7 April 2009.
Kulier R, Kapp N, Gülmezoglu AM, Hofmeyr GJ, Cheng L, Campana A (2011). "Medical methods for first trimester abortion". The Cochrane Database of Systematic Reviews. 11 (11): CD002855. doi:10.1002/14651858.CD002855.pub4. PMID 22071804.
Creinin MD, Gemzell-Danielsson K (2009). "Medical abortion in early pregnancy". In Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD. Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell. pp. 111–134. ISBN 1-4051-7696-2.
Kapp N, von Hertzen H (2009). "Medical methods to induce abortion in the second trimester". In Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD. Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell. pp. 178–192. ISBN 1-4051-7696-2.
Wildschut, H; Both, MI; Medema, S; Thomee, E; Wildhagen, MF; Kapp, N (19 January 2011). "Medical methods for mid-trimester termination of pregnancy". The Cochrane Database of Systematic Reviews (1): CD005216. doi:10.1002/14651858.CD005216.pub2. PMID 21249669.
Chen, MJ; Creinin, MD (July 2015). "Mifepristone With Buccal Misoprostol for Medical Abortion: A Systematic Review". Obstetrics and Gynecology. 126 (1): 12–21. doi:10.1097/AOG.0000000000000897. PMID 26241251.
WHO Department of Reproductive Health and Research (23 November 2006). Frequently asked clinical questions about medical abortion (PDF). Geneva: World Health Organization. ISBN 92-4-159484-5. Archived (PDF) from the original on 26 December 2011. Retrieved 22 November 2011.(subscription required)
Fjerstad M, Sivin I, Lichtenberg ES, Trussell J, Cleland K, Cullins V (September 2009). "Effectiveness of medical abortion with mifepristone and buccal misoprostol through 59 gestational days". Contraception. 80 (3): 282–286. doi:10.1016/j.contraception.2009.03.010. PMC 3766037. PMID 19698822. The regimen (200 mg of mifepristone, followed 24–48 hours later by 800 mcg of vaginal misoprostol) previously used by Planned Parenthood clinics in the United States from 2001 to March 2006 was 98.5% effective through 63 days gestation—with an ongoing pregnancy rate of about 0.5%, and an additional 1% of women having uterine evacuation for various reasons, including problematic bleeding, persistent gestational sac, clinician judgment or a woman's request. The regimen (200 mg of mifepristone, followed 24–48 hours later by 800 mcg of buccal misoprostol) currently used by Planned Parenthood clinics in the United States since April 2006 is 98.3% effective through 59 days gestation.
Holmquist S, Gilliam M (2008). "Induced abortion". In Gibbs RS, Karlan BY, Haney AF, Nygaard I. Danforth's obstetrics and gynecology (10th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 586–603. ISBN 978-0-7817-6937-2.
"Abortion statistics, England and Wales: 2010" (PDF). London: Department of Health, United Kingdom. 24 May 2011. Retrieved 22 November 2011.
"Abortion statistics, year ending 31 December 2010" (PDF). Edinburgh: ISD, NHS Scotland. 31 May 2011. Archived (PDF) from the original on 26 July 2011. Retrieved 22 November 2011.
Vilain A, Mouquet MC (22 June 2011). "Voluntary terminations of pregnancies in 2008 and 2009" (PDF). Paris: DREES, Ministry of Health, France. Archived from the original (PDF) on 26 September 2011. Retrieved 22 November 2011.
. (5 July 2011). "Abortions in Switzerland 2010". Neuchatel: Office of Federal Statistics, Switzerland. Archived from the original on 3 October 2011. Retrieved 22 November 2011.
Gissler M, Heino A (21 February 2011). "Induced abortions in the Nordic countries 2009" (PDF). Helsinki: National Institute for Health and Welfare, Finland. Archived from the original (PDF) on 18 January 2012. Retrieved 22 November 2011.
Jones, Rachel K.; Jerman, Jenna (January 17, 2017). "Abortion incidence and service availability in the United States, 2014". Perspectives on Sexual and Reproductive Health. 49 (1): 17–27. doi:10.1363/psrh.12015. PMC 5487028. PMID 28094905.
96% of all abortions performed in nonhospital facilities × 31% early medical abortions of all nonhospital abortions = 30% early medical abortions of all abortions; 97% of nonhospital medical abortions used mifepristone and misoprostol—3% used methotrexate and misoprostol, or misoprostol alone—in the United States in 2014.
Hammond C, Chasen ST (2009). "Dilation and evacuation". In Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD. Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford: Wiley-Blackwell. pp. 178–192. ISBN 1-4051-7696-2.
Healthwise (2004). "Manual and vacuum aspiration for abortion". WebMD. Archived from the original on 11 February 2007. Retrieved 5 December 2008.
World Health Organization (2003). "Dilatation and curettage". Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors. Geneva: World Health Organization. ISBN 978-92-4-154587-7. OCLC 181845530. Retrieved 5 December 2008.
McGee, Glenn; Jon F. Merz. "Abortion". Encarta. Microsoft. Archived from the original on 31 October 2009. Retrieved 5 December 2008.
Templeton, A.; Grimes, D. A. (2011). "A Request for Abortion". New England Journal of Medicine. 365 (23): 2198–2204. doi:10.1056/NEJMcp1103639. Archived from the original on 8 January 2012.
Borgatta, L (December 2014). "Labor Induction Termination of Pregnancy". Global Library of Women's Medicine. GLOWM.10444. doi:10.3843/GLOWM.10444. Archived from the original on 24 September 2015. Retrieved 25 September 2015.
Society of Family Planning (February 2011). "Clinical Guidelines, Labor induction abortion in the second trimester". Contraception. 84 (1): 4–18. doi:10.1016/j.contraception.2011.02.005. Retrieved 25 September 2015. 10. What is the effect of feticide on labor induction abortion outcome? Deliberately causing demise of the fetus before labor induction abortion is performed primarily to avoid transient fetal survival after expulsion; this approach may be for the comfort of both the woman and the staff, to avoid futile resuscitation efforts. Some providers allege that feticide also facilitates delivery, although little data support this claim. Transient fetal survival is very unlikely after intraamniotic installation of saline or urea, which are directly feticidal. Transient survival with misoprostol for labor induction abortion at greater than 18 weeks ranges from 0% to 50% and has been observed in up to 13% of abortions performed with high-dose oxytocin. Factors associated with a higher likelihood of transient fetal survival with labor induction abortion include increasing gestational age, decreasing abortion interval and the use of nonfeticidal inductive agents such as the PGE1 analogues.
"2015 Clinical Policy Guidelines" (PDF). National Abortion Federation. 2015. Archived (PDF) from the original on 12 August 2015. Retrieved 30 October 2015. Policy Statement: Medical induction abortion is a safe and effective method for termination of pregnancies beyond the first trimester when performed by trained clinicians in medical offices, freestanding clinics, ambulatory surgery centers, and hospitals. Feticidal agents may be particularly important when issues of viability arise.
Riddle, John M. (1997). Eve's herbs: a history of contraception and abortion in the West. Cambridge, Massachusetts: Harvard University Press. ISBN 978-0-674-27024-4. OCLC 36126503.
Sullivan, John B.; Rumack, Barry H.; Thomas, Harold Jr; et al. (1979), "Pennyroyal oil poisoning and hepatoxicity", Journal of the American Medical Association, 242 (26): 2873–2874, doi:10.1001/jama.1979.03300260043027
Ciganda C, Laborde A (2003). "Herbal infusions used for induced abortion". Journal of Toxicology: Clinical Toxicology. 41 (3): 235–239. doi:10.1081/CLT-120021104. PMID 12807304.
Smith JP (1998). "Risky choices: The dangers of teens using self-induced abortion attempts". Journal of Pediatric Health Care. 12 (3): 147–151. doi:10.1016/S0891-5245(98)90245-0. PMID 9652283.
Potts, M.; Graff, M.; Taing, J. (2007). "Thousand-year-old depictions of massage abortion". Journal of Family Planning and Reproductive Health Care. 33 (4): 233–234. doi:10.1783/147118907782101904. PMID 17925100.
Thapa, S. R.; Rimal, D.; Preston, J. (2006). "Self induction of abortion with instrumentation". Australian Family Physician. 35 (9): 697–698. PMID 16969439. Archived from the original on 8 January 2009.
"The Prevention and Management of Unsafe Abortion" (PDF). World Health Organization. April 1992. Archived (PDF) from the original on 30 May 2010. Retrieved 18 October 2017.
Grimes, DA; Creinin, MD (2004). "Induced abortion: an overview for internists". Annals of Internal Medicine. 140 (8): 620–6. doi:10.7326/0003-4819-140-8-200404200-00009. PMID 15096333. Archived from the original on 7 May 2010.
Raymond, E. G.; Grimes, D. A. (2012). "The Comparative Safety of Legal Induced Abortion and Childbirth in the United States". Obstetrics & Gynecology. 119 (2, Part 1): 215–219. doi:10.1097/AOG.0b013e31823fe923. PMID 22270271.
Grimes DA (January 2006). "Estimation of pregnancy-related mortality risk by pregnancy outcome, United States, 1991 to 1999". American Journal of Obstetrics & Gynecology. 194 (1): 92–4. doi:10.1016/j.ajog.2005.06.070. PMID 16389015.
Raymond, EG; Grossman, D; Weaver, MA; Toti, S; Winikoff, B (November 2014). "Mortality of induced abortion, other outpatient surgical procedures and common activities in the United States". Contraception. 90 (5): 476–9. doi:10.1016/j.contraception.2014.07.012. PMID 25152259.
Bartlett LA; Berg CJ; Shulman HB; et al. (April 2004). "Risk factors for legal induced abortion-related mortality in the United States". Obstetrics & Gynecology. 103 (4): 729–37. doi:10.1097/01.AOG.0000116260.81570.60. PMID 15051566.
Trupin, Suzanne (27 May 2010). "Elective Abortion". eMedicine. Archived from the original on 14 December 2004. Retrieved 1 June 2010. At every gestational age, elective abortion is safer for the mother than carrying a pregnancy to term.
Pittman, Genevra (23 January 2012). "Abortion safer than giving birth: study". Reuters. Archived from the original on 6 February 2012. Retrieved 4 February 2012.
Abbas, D; Chong, E; Raymond, EG (September 2015). "Outpatient medical abortion is safe and effective through 70 days gestation". Contraception. 92 (3): 197–9. doi:10.1016/j.contraception.2015.06.018. PMID 26118638.
Kapp, Nathalie; Baldwin, Maureen K.; Rodriguez, Maria Isabel (2017-09-18). "Efficacy of medical abortion prior to 6 gestational weeks: a systematic review". Contraception. 97: 90–99. doi:10.1016/j.contraception.2017.09.006. ISSN 1879-0518. PMID 28935220.
Westfall JM, Sophocles A, Burggraf H, Ellis S (1998). "Manual vacuum aspiration for first-trimester abortion". Arch Fam Med. 7 (6): 559–62. doi:10.1001/archfami.7.6.559. PMID 9821831. Archived from the original on 5 April 2005.
Dempsey, A (December 2012). "Serious infection associated with induced abortion in the United States". Clinical Obstetrics and Gynecology. 55 (4): 888–92. doi:10.1097/GRF.0b013e31826fd8f8. PMID 23090457.
White, Kari; Carroll, Erin; Grossman, Daniel (November 2015). "Complications from first-trimester aspiration abortion: a systematic review of the literature". Contraception. 92 (5): 422–438. doi:10.1016/j.contraception.2015.07.013. PMID 26238336.
ACOG Committee on Practice Bulletins—Gynecology (May 2009). "ACOG practice bulletin No. 104: antibiotic prophylaxis for gynecologic procedures". Obstetrics & Gynecology. 113 (5): 1180–9. doi:10.1097/AOG.0b013e3181a6d011. PMID 19384149.
Sawaya GF, Grady D, Kerlikowske K, Grimes DA (May 1996). "Antibiotics at the time of induced abortion: the case for universal prophylaxis based on a meta-analysis". Obstetrics & Gynecology. 87 (5 Pt 2): 884–90. PMID 8677129.
Barnard, S; Kim, C; Park, MH; Ngo, TD (27 July 2015). "Doctors or mid-level providers for abortion". The Cochrane Database of Systematic Reviews (7): CD011242. doi:10.1002/14651858.CD011242.pub2. PMID 26214844.
Lerma, Klaira; Shaw, Kate A. (2017-09-15). "Update on second trimester medical abortion". Current Opinion in Obstetrics and Gynecology. 29: 413–418. doi:10.1097/GCO.0000000000000409. ISSN 1473-656X. PMID 28922193.
Grossman D (3 September 2004). "Medical methods for first trimester abortion: RHL commentary". Reproductive Health Library. Geneva: World Health Organization. Archived from the original on 28 October 2011. Retrieved 22 November 2011.
Chien P, Thomson M (15 December 2006). "Medical versus surgical methods for first trimester termination of pregnancy: RHL commentary". Reproductive Health Library. Geneva: World Health Organization. Archived from the original on 17 May 2010. Retrieved 1 June 2010.
Jasen P (October 2005). "Breast cancer and the politics of abortion in the United States". Medical History. 49 (4): 423–44. doi:10.1017/S0025727300009145. PMC 1251638. PMID 16562329.
Schneider, A. Patrick II; Zainer, Christine; et al. (August 2014). "The breast cancer epidemic: 10 facts". The Linacre Quarterly. Catholic Medical Association. 81 (3): 244–277. doi:10.1179/2050854914Y.0000000027. PMC 4135458. Retrieved 11 November 2015. an association between [induced abortion] and breast cancer has been found by numerous Western and non-Western researchers from around the world. This is especially true in more recent reports that allow for a sufficient breast cancer latency period since an adoption of a Western life style in sexual and reproductive behavior.
Position statements of major medical bodies on abortion and breast cancer include:
World Health Organization: "Induced abortion does not increase breast cancer risk (Fact sheet N°240)". World Health Organization. Archived from the original on 13 February 2011. Retrieved 6 January 2011.
National Cancer Institute: "Abortion, Miscarriage, and Breast Cancer Risk". National Cancer Institute. Archived from the original on 21 December 2010. Retrieved 11 January 2011.
American Cancer Society: "Is Abortion Linked to Breast Cancer?". American Cancer Society. 23 September 2010. Archived from the original on 5 June 2011. Retrieved 20 June 2011. At this time, the scientific evidence does not support the notion that abortion of any kind raises the risk of breast cancer.
Royal College of Obstetricians and Gynaecologists: "The Care of Women Requesting Induced Abortion" (PDF). Royal College of Obstetricians and Gynaecologists. p. 9. Archived from the original (PDF) on 27 July 2013. Retrieved 29 June 2008. Induced abortion is not associated with an increase in breast cancer risk.
American Congress of Obstetricians and Gynecologists: "ACOG Finds No Link Between Abortion and Breast Cancer Risk". American Congress of Obstetricians and Gynecologists. 31 July 2003. Archived from the original on 2 January 2011. Retrieved 11 January 2011.
Gordon, Linda (2002). The Moral Property of Women. University of Illinois Press. ISBN 0252027647.
Solinger, Rickie (1998), "Introduction", in Solinger, Rickie, Abortion Wars: A Half Century of Struggle, 1950-2000, University of California Press, pp. 1–9, ISBN 978-0520209527
Bates, Jerome E.; Zawadzki, Edward S. (1964). Criminal Abortion: A Study in Medical Sociology. Charles C. Thomas. ISBN 9780398001094.
Keller, Allan (1981). Scandalous Lady: The Life and Times of Madame Restell. Atheneum. ISBN 978-0689112133.
Taussig, Frederick J. (1936). Abortion Spontaneous and Induced: Medical and Social Aspects. C. V. Mosby.
Horvath, S; Schreiber, CA (14 September 2017). "Unintended Pregnancy, Induced Abortion, and Mental Health". Current Psychiatry Reports. 19 (11): 77. doi:10.1007/s11920-017-0832-4. PMID 28905259.
"APA Task Force Finds Single Abortion Not a Threat to Women's Mental Health" (Press release). American Psychological Association. 12 August 2008. Archived from the original on 6 September 2011. Retrieved 7 September 2011.
"Report of the APA Task Force on Mental Health and Abortion" (PDF). Washington, DC: American Psychological Association. 13 August 2008. Archived (PDF) from the original on 15 June 2010.
Coleman, PK (September 2011). "Abortion and mental health: quantitative synthesis and analysis of research published 1995-2009". The British Journal of Psychiatry. 199 (3): 180–6. doi:10.1192/bjp.bp.110.077230. PMID 21881096.
"Mental Health and Abortion". American Psychological Association. 2008. Archived from the original on 19 April 2012. Retrieved 18 April 2012.
Steinberg, J. R. (2011). "Later Abortions and Mental Health: Psychological Experiences of Women Having Later Abortions—A Critical Review of Research". Women's Health Issues. 21 (3): S44–S48. doi:10.1016/j.whi.2011.02.002. PMID 21530839.
Kelly, Kimberly (February 2014). "The spread of 'Post Abortion Syndrome' as social diagnosis". Social Science & Medicine. 102: 18–25. doi:10.1016/j.socscimed.2013.11.030.
Okonofua, F. (2006). "Abortion and maternal mortality in the developing world" (PDF). Journal of Obstetrics and Gynaecology Canada. 28 (11): 974–979. PMID 17169222. Archived from the original (PDF) on 11 January 2012.
Haddad, LB.; Nour, NM. (2009). "Unsafe abortion: unnecessary maternal mortality". Reviews in Obstetrics & Gynecology. 2 (2): 122–6. PMC 2709326. PMID 19609407.
Lozano, R (15 December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604.
Darney, Leon Speroff, Philip D. (2010). A clinical guide for contraception (5th ed.). Philadelphia, Pa.: Lippincott Williams & Wilkins. p. 406. ISBN 1-60831-610-6.
World Health Organisation (2011). Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008 (PDF) (6th ed.). World Health Organisation. p. 27. ISBN 978-92-4-150111-8. Archived (PDF) from the original on 28 March 2014.
Berer M (2000). "Making abortions safe: a matter of good public health policy and practice". Bulletin of the World Health Organization. 78 (5): 580–92. PMC 2560758. PMID 10859852.
"Translations". Dublin Declaration. Archived from the original on 28 October 2015. Retrieved 28 October 2015.
Sedgh G, Henshaw S, Singh S, Ahman E, Shah IH (2007). "Induced abortion: estimated rates and trends worldwide". Lancet. 370 (9595): 1338–45. CiteSeerX 10.1.1.454.4197. doi:10.1016/S0140-6736(07)61575-X. PMID 17933648.
"Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003" (PDF). World Health Organization. 2007. Archived (PDF) from the original on 16 February 2011. Retrieved 7 March 2011.
Berer M (November 2004). "National laws and unsafe abortion: the parameters of change". Reproductive Health Matters. 12 (24 Suppl): 1–8. doi:10.1016/S0968-8080(04)24024-1. PMID 15938152.
Culwell, Kelly R.; Hurwitz, Manuelle (May 2013). "Addressing barriers to safe abortion". International Journal of Gynecology & Obstetrics. 121: S16–S19. doi:10.1016/j.ijgo.2013.02.003.
Jewkes R, Rees H, Dickson K, Brown H, Levin J (March 2005). "The impact of age on the epidemiology of incomplete abortions in South Africa after legislative change". BJOG: An International Journal of Obstetrics & Gynaecology. 112 (3): 355–9. doi:10.1111/j.1471-0528.2004.00422.x. PMID 15713153.
Bateman C (December 2007). "Maternal mortalities 90% down as legal TOPs more than triple". South African Medical Journal. 97 (12): 1238–42. PMID 18264602. Archived from the original on 30 August 2017.
Conti, Jennifer A.; Brant, Ashley R.; Shumaker, Heather D.; Reeves, Matthew F. (November 2016). "Update on abortion policy". Current Opinion in Obstetrics and Gynecology: 1. doi:10.1097/GCO.0000000000000324.
New, M. J. (15 February 2011). "Analyzing the Effect of Anti-Abortion U.S. State Legislation in the Post-Casey Era". State Politics & Policy Quarterly. 11 (1): 28–47. doi:10.1177/1532440010387397.
Medoff, M. H.; Dennis, C. (21 July 2014). "Another Critical Review of New's Reanalysis of the Impact of Antiabortion Legislation". State Politics & Policy Quarterly. 14 (3): 269–276. doi:10.1177/1532440014535476.
"Facts on Investing in Family Planning and Maternal and Newborn Health" (PDF). Guttmacher Institute. 2010. Archived from the original (PDF) on 24 March 2012. Retrieved 24 May 2012.
Grimes, David A. "Unsafe Abortion - The Preventable Pandemic*". Archived from the original on 5 March 2014. Retrieved 16 January 2010.
Nations, MK (1997). "Women's hidden transcripts about abortion in Brazil". Social Science & Medicine. 44: 1833–45. doi:10.1016/s0277-9536(96)00293-6. PMID 9194245.
Maclean, Gaynor (2005). "XI. Dimension, Dynamics and Diversity: A 3D Approach to Appraising Global Maternal and Neonatal Health Initiatives". In Balin, Randell E. Trends in Midwifery Research. Nova Publishers. pp. 299–300. ISBN 978-1-59454-477-4. Archived from the original on 15 March 2015.
Salter, C.; Johnson, H.B.; Hengen, N. (1997). "Care for Postabortion Complications: Saving Women's Lives". Population Reports. Johns Hopkins School of Public Health. 25 (1). Archived from the original on 7 December 2009.
UNICEF, United Nations Population Fund, WHO, World Bank (2010). "Packages of interventions: Family planning, safe abortion care, maternal, newborn and child health". Archived from the original on 9 November 2010. Retrieved 31 December 2010.
"The Care of Women Requesting Induced Abortion. Evidence-Based Clinical Guideline no. 7" (PDF). Royal College of Obstetricians and Gynaecologists. November 2011. Archived (PDF) from the original on 14 November 2015. Retrieved 31 October 2015. RECOMMENDATION 6.21 Feticide should be performed before medical abortion after 21 weeks and 6 days of gestation to ensure that there is no risk of a live birth.
Society of Family Planning (February 2011). "Clinical Guidelines, Labor induction abortion in the second trimester". Contraception. 84 (1): 4–18. doi:10.1016/j.contraception.2011.02.005. Transient survival with misoprostol for labor induction abortion at greater than 18 weeks ranges from 0% to 50% and has been observed in up to 13% of abortions performed with high-dose oxytocin.
Fletcher; Isada; Johnson; Evans (August 1992). "Fetal intracardiac potassium chloride injection to avoid the hopeless resuscitation of an abnormal abortus: II. Ethical issues". Obstetrics and Gynecology. 80 (2): 310–313. PMID 1635751. following later abortions at greater than 20 weeks, the rare but catastrophic occurrence of live births can lead to fractious controversy over neonatal management.
"Termination of Pregnancy for Fetal Abnormality" (PDF). Royal College of Obstetricians and Gynaecologists: 29–31. May 2010. Archived (PDF) from the original on 22 December 2015. Retrieved 26 October 2015.
Nuffield Council on Bioethics (2007). "Critical care decisions in fetal and neonatal medicine: a guide to the report" (PDF). Archived (PDF) from the original on 4 March 2016. Retrieved 29 October 2015. Under English law, fetuses have no independent legal status. Once born, babies have the same rights to life as other people.
Gerri R. Baer; Robert M. Nelson (2007). "Preterm Birth: Causes, Consequences, and Prevention. C: A Review of Ethical Issues Involved in Premature Birth". Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes;. Archived from the original on 31 December 2015. In 2002, the 107th U.S. Congress passed the Born-Alive Infants Protection Act of 2001. This law established personhood for all infants who are born "at any stage of development" who breathe, have a heartbeat, or "definite movement of voluntary muscles", regardless of whether the birth was due to labor or induced abortion.
Chabot, Steve (5 August 2002). "H.R. 2175 (107th): Born-Alive Infants Protection Act of 2002". govtrack.us. Archived from the original on 14 November 2015. Retrieved 30 October 2015. The term "born alive" is defined as the complete expulsion or extraction from its mother of that member, at any stage of development, who after such expulsion or extraction breathes or has a beating heart, pulsation of the umbilical cord, or definite movement of the voluntary muscles, regardless of whether the umbilical cord has been cut, and regardless of whether the expulsion or extraction occurs as a result of natural or induced labor, cesarean section, or induced abortion.
"Practice Bulletin: Second-Trimester Abortion" (PDF). Obstetrics & Gynecology. 121 (6): 1394–1406. June 2013. doi:10.1097/01.AOG.0000431056.79334.cc. PMID 23812485. Archived (PDF) from the original on 14 November 2015. Retrieved 30 October 2015. With medical abortion after 20 weeks of gestation, induced fetal demise may be preferable to the woman or provider in order to avoid transient fetal survival after expulsion.
Higginbotham Susan (January 2010). "Clinical Guidelines: Induction of fetal demise before abortion" (PDF). Contraception: a publication of Society of Family Planning. 81: 8. doi:10.1016/j.contraception.2010.01.018. Archived (PDF) from the original on 23 November 2015. Retrieved 26 October 2015. Inducing fetal demise before induction termination avoids signs of live birth that may have beneficial emotional, ethical and legal consequences.
Committee on Health Care for Underserved Women (November 2014). "Committee Opinion 613: Increasing Access to Abortion". Obstetrics & Gynecology. 124: 1060–1065. doi:10.1097/01.aog.0000456326.88857.31. Archived from the original on 28 October 2015. Retrieved 28 October 2015. "Partial-birth" abortion bans—The federal Partial-Birth Abortion Ban Act of 2003 (upheld by the Supreme Court in 2007) makes it a federal crime to perform procedures that fall within the definition of so-called "partial-birth abortion" contained in the statute, with no exception for procedures necessary to preserve the health of the woman...physicians and lawyers have interpreted the banned procedures as including intact dilation and evacuation unless fetal demise occurs before surgery.
"2015 Clinical Policy Guidelines" (PDF). National Abortion Federation. 2015. Archived (PDF) from the original on 12 August 2015. Retrieved 30 October 2015. Policy Statement: Medical induction abortion is a safe and effective method for termination of pregnancies beyond the first trimester when performed by trained clinicians in medical offices, freestanding clinics, ambulatory surgery centers, and hospitals. Feticidal agents may be particularly important when issues of viability arise.
Milliez Jacques (2008). "FIGO (International Federation of Gynecology and Obstetrics) Committee Report: Ethical aspects concerning termination of pregnancy following prenatal diagnosis". International Journal of Gynecology and Obstetrics. 102 (1): 97–98. doi:10.1016/j.ijgo.2008.03.002. PMID 18423641. Termination of pregnancy following prenatal diagnosis after 22 weeks must be preceded by a feticide
"Underlying Cause of Death 1999-2013 on CDC WONDER Online Database, released 2015". Centers for Disease Control and Prevention, National Center for Health Statistics. Data are from the Multiple Cause of Death Files, 1999–2013, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Archived from the original on 14 November 2015. Retrieved 12 November 2015.
Pazol, Karen; et al. (27 November 2009). "Abortion Surveillance - United States, 2006". Morbidity and Mortality Weekly Report Surveillance Summaries. 58 (SS08): 1–35. Archived from the original on 28 November 2015. Retrieved 12 November 2015.
Shah I, Ahman E (December 2009). "Unsafe abortion: global and regional incidence, trends, consequences, and challenges". Journal of Obstetrics and Gynaecology Canada. 31 (12): 1149–58. doi:10.1016/s1701-2163(16)34376-6. PMID 20085681. However, a woman's chance of having an abortion is similar whether she lives in a developed or a developing region: in 2003 the rates were 26 abortions per 1000 women aged 15 to 44 in developed areas and 29 per 1000 in developing areas. The main difference is in safety, with abortion being safe and easily accessible in developed countries and generally restricted and unsafe in most developing countries
Rosenthal, Elizabeth (12 October 2007). "Legal or Not, Abortion Rates Compare". The New York Times. Archived from the original on 28 August 2011. Retrieved 18 July 2011.
"Facts on Investing in Family Planning and Maternal and Newborn Health" (PDF). Guttmacher Institute. November 2010. Archived from the original (PDF) on 20 October 2011. Retrieved 24 October 2011.
Sedgh, G.; Singh, S.; Henshaw, S. K.; Bankole, A. (2011). "Legal Abortion Worldwide in 2008: Levels and Recent Trends". Perspectives on Sexual and Reproductive Health. 43 (3): 188–198. doi:10.1363/4318811. PMID 21884387. Archived from the original on 7 January 2012.
National Institute of Statistics, Romanian Statistical Yearbook, chapter 2, page 62, 2011
Strauss, L. T.; Gamble, S. B.; Parker, W. Y.; Cook, D. A.; Zane, S. B.; Hamdan, S.; Centers for Disease Control Prevention (2006). "Abortion surveillance—United States, 2003". Morbidity and Mortality Weekly Report Surveillance Summaries. 55 (SS11): 1–32. PMID 17119534. Archived from the original on 2 June 2017.
"The limitations of U.S. statistics on abortion". Issues in Brief. New York: The Guttmacher Institute. 1997. Archived from the original on 4 April 2012.
Finer, L. B.; Henshaw, S. K. (2003). "Abortion Incidence and Services in the United States in 2000". Perspectives on Sexual and Reproductive Health. 35 (1): 6–15. doi:10.1363/3500603. PMID 12602752. Archived from the original on 22 January 2016.
Department of Health (2007). "Abortion statistics, England and Wales: 2006". Archived from the original on 6 December 2010. Retrieved 12 October 2007.
Cheng, Linan (1 November 2008). "Surgical versus medical methods for second-trimester induced abortion: RHL commentary". The WHO Reproductive Health Library. Geneva: World Health Organization. Archived from the original on 15 February 2009. Retrieved 10 February 2009. commentary on:
Lohr, Patricia A.; Hayes, Jennifer L.; Gemzell-Danielsson, Kristina (23 January 2008). "Surgical versus medical methods for second trimester abortion". The Cochrane Database of Systematic Reviews (1): CD006714. doi:10.1002/14651858.CD006714.pub2. PMID 18254113.
Bankole, Akinrinola; Singh, Susheela; Haas, Taylor (1998). "Reasons Why Women Have Induced Abortions: Evidence from 27 Countries". International Family Planning Perspectives. 24 (3): 117–127, 152. doi:10.2307/3038208. Archived from the original on 17 January 2006.
Finer, L. B.; Frohwirth, L. F.; Dauphinee, L. A.; Singh, S.; Moore, A. M. (2005). "Reasons U.S. Women Have Abortions: Quantitative and Qualitative Perspectives". Perspectives on Sexual and Reproductive Health. 37 (3): 110–118. doi:10.1111/j.1931-2393.2005.tb00045.x. PMID 16150658. Archived from the original on 7 January 2012.
"Nuremberg and the Crime of Abortion". U. Toledo. L. Rev. 42: 283. Archived from the original on 3 November 2013. Retrieved 12 July 2014.
Oster, Emily (September 2005). "Explaining Asia's "Missing Women": A New Look at the Data – Comment" (PDF). Population and Development Review. 31 (3): 529, 535. doi:10.1111/j.1728-4457.2005.00082.x. Archived from the original (PDF) on 30 August 2008. Retrieved 19 May 2009.
Jones, R. K.; Darroch, J. E.; Henshaw, S. K. (2002). "Contraceptive Use Among U.S. Women Having Abortions in 2000–2001" (PDF). Perspectives on Sexual and Reproductive Health. 34 (6): 294–303. doi:10.2307/3097748. PMID 12558092. Archived (PDF) from the original on 15 June 2006.
Cohen, SA (2008). "Abortion and Women of Color: The Bigger Picture". Guttmacher Policy Review. 11 (3). Archived from the original on 15 September 2008.
George J. Annas and Sherman Elias. Legal and Ethical Issues in Obstetrical Practice. Chapter 54 in Obstetrics: Normal and Problem Pregnancies, 6th edition. Eds. Steven G. Gabbe, et al. 2012 Saunders, an imprint of Elsevier. ISBN 978-1-4377-1935-2
Doan 2007, p. 57.
Weisz, B; Schiff, E; Lishner, M (2001). "Cancer in pregnancy: maternal and fetal implications" (PDF). Human Reproduction Update. 7 (4): 384–393. doi:10.1093/humupd/7.4.384. PMID 11476351. Archived (PDF) from the original on 15 October 2015.
Mayr, NA; Wen, BC; Saw, CB (1998). "Radiation therapy during pregnancy". Obstetrics & Gynecology Clinics of North America. 25 (2): 301–21. doi:10.1016/s0889-8545(05)70006-1. PMID 9629572.
Fenig E, Mishaeli M, Kalish Y, Lishner M (2001). "Pregnancy and radiation". Cancer Treatment Reviews. 27 (1): 1–7. doi:10.1053/ctrv.2000.0193. PMID 11237773.
Li WW, Yau TN, Leung CW, Pong WM, Chan MY (2009). "Large-cell neuroendocrine carcinoma of the uterine cervix complicating pregnancy". Hong Kong Medical Journal. 15 (1): 69–72. PMID 19197101.
Mould R (1996). Mould's Medical Anecdotes. CRC Press. p. 406. ISBN 978-0-85274-119-1.
Miles, Steven (2005). The Hippocratic Oath and the Ethics of Medicine. Oxford University Press. ISBN 978-0-19-518820-2.
"Scribonius Largus and the Oath of Hippocrates". penelope.uchicago.edu.
Soranus, Owsei Temkin (1956). Soranus' Gynecology. I.19.60: JHU Press. Archived from the original on 15 October 2015. Retrieved 6 October 2015.
Carrick, Paul (2001). Medical Ethics in the Ancient World. Georgetown University Press. ISBN 978-0-87840-849-8.
Rackham, H. (1944). "Aristotle, Politics". Harvard University Press. Archived from the original on 22 June 2011. Retrieved 21 June 2011.
Brind'Amour, Katherine (2007). "Effraenatam". Embryo Project Encyclopedia. Arizona State University. Archived from the original on 2 February 2012.
Joan Cadden, "Western medicine and natural philosophy," in Vern L. Bullough and James A. Brundage, eds., Handbook of Medieval Sexuality, Garland, 1996, p. 51-80.
Cyril C. Means, Jr., "A historian's view," in Robert E. Hall, ed., Abortion in a Changing World, vol. 1, Columbia University Press, 1970, p. 16-24.
John M. Riddle, "Contraception and early abortion in the Middle Ages," in Vern L. Bullough and James A. Brundage, eds., Handbook of Medieval Sexuality, Garland, 1996, pp. 261-277, ISBN 9780815312871.
"Religions – Islam: Abortion". BBC. Archived from the original on 9 October 2011. Retrieved 10 December 2011.
Dabash, Rasha; Roudi-Fahimi, Farzaneh (2008). "Abortion in the Middle East and North Africa" (PDF). Population Research Bureau. Archived (PDF) from the original on 6 October 2011.
Dannenfelser, Marjorie (4 November 2015). "The Suffragettes Would Not Agree With Feminists Today on Abortion". TIME. Archived from the original on 6 November 2015. Retrieved 4 November 2015.
Charles A. Lee, "Report of a trial for murder," American Journal of the Medical Sciences, vol. XXII (1838), p. 351-353.
Benjamin Bailey, "Induction of abortion and premature labor," North American Journal of Homeopathy, vol. XI, no. 3 (1896), p. 144-150.
Keith Simpson, Forensic Medicine, Edward Arnold Publishers, 1969 [first published 1947], p. 173-174.
Leslie J. Reagan, When Abortion Was a Crime: Women, Medicine, and Law in the United States, 1867-1973, University of California Press, 1997.
Max Evans, Madam Millie: Bordellos from Silver City to Ketchikan, University of New Mexico Press, 2002, p. 209-218, 230, 267-286, 305.
James Donner, Women in Trouble: The Truth about Abortion in America, Monarch Books, 1959.
Ann Oakley, The Captured Womb, Basil Blackwell, 1984, p. 91.
Rickie Solinger, The Abortionist: A Woman Against the Law, The Free Press, 1994, p. xi, 5, 16-17, 157-175.
"Abortion Law, History & Religion". Childbirth By Choice Trust. Archived from the original on 12 January 2013. Retrieved 23 March 2008.
For sources describing abortion policy in Nazi Germany, see:
Friedlander, Henry (1995). The origins of Nazi genocide: from euthanasia to the final solution. Chapel Hill: University of North Carolina Press. p. 30. ISBN 978-0-8078-4675-9. OCLC 60191622. Archived from the original on 29 July 2016.
Proctor, Robert (1988). Racial Hygiene: Medicine Under the Nazis. Cambridge, Massachusetts: Harvard University Press. pp. 122, 123 and 366. ISBN 978-0-674-74578-0. OCLC 20760638.
Arnot, Margaret L.; Cornelie Usborne (1999). Gender and Crime in Modern Europe. New York: Routledge. p. 231. ISBN 978-1-85728-745-5. OCLC 186748539.
DiMeglio, Peter M. (1999). "Germany 1933–1945 (National Socialism)". In Helen Tierney. Women's studies encyclopedia. Westport, Connecticut: Greenwood Press. p. 589. ISBN 978-0-313-31072-0. OCLC 38504469. Archived from the original on 15 October 2015.
Farrell, Courtney (2010). Abortion Debate. ABDO Publishing Company. pp. 6–7. ISBN 1617852643.
"WMA Declaration on Therapeutic Abortion". WMA. Archived from the original on 28 October 2015. Retrieved 28 October 2015.
Farrell, p. 8
"World Abortion Policies 2013" (PDF). United Nations Department of Economic and Social Affairs, Population Division. Retrieved 31 July 2013.
World Abortion Policies 2007, United Nations, Department of Economic and Social Affairs, Population Division.
Theodore J. Joyce; Stanley K. Henshaw; Amanda Dennis; Lawrence B. Finer; Kelly Blanchard (April 2009). "The Impact of State Mandatory Counseling and Waiting Period Laws on Abortion: A Literature Review" (PDF). Guttmacher Institute. Archived from the original (PDF) on 14 January 2011. Retrieved 31 December 2010.
Phillips, Tom (29 October 2015). "China ends one-child policy after 35 years". The Guardian. ISSN 0261-3077. Archived from the original on 1 December 2016. Retrieved 30 November 2016.
Buckley, Chris (29 October 2015). "China Ends One-Child Policy, Allowing Families Two Children". The New York Times. ISSN 0362-4331. Archived from the original on 24 November 2016. Retrieved 30 November 2016.
"China to end one-child policy and allow two". BBC News. 29 October 2015. Archived from the original on 21 November 2016. Retrieved 30 November 2016.
Restivo, Sal P., ed. (2005). Science, Technology, and Society: An Encyclopedia. Oxford University Press. p. 2. ISBN 9780195141931. Archived from the original on 15 March 2015.
"European delegation visits Nicaragua to examine effects of abortion ban". Ipas. 26 November 2007. Archived from the original on 17 April 2008. Retrieved 15 June 2009. More than 82 maternal deaths had been registered in Nicaragua since the change. During this same period, indirect obstetric deaths, or deaths caused by illnesses aggravated by the normal effects of pregnancy and not due to direct obstetric causes, have doubled.
"Nicaragua: "The Women's Movement Is in Opposition"". Montevideo: Inside Costa Rica. IPS. 28 June 2008. Archived from the original on 6 June 2011.
"Surgical Abortion: History and Overview". National Abortion Federation. Archived from the original on 22 September 2006. Retrieved 4 September 2006.
Nations MK, Misago C, Fonseca W, Correia LL, Campbell OM (June 1997). "Women's hidden transcripts about abortion in Brazil". Social Science & Medicine. 44 (12): 1833–45. doi:10.1016/s0277-9536(96)00293-6. PMID 9194245. Two folk medical conditions, "delayed" (atrasada) and "suspended" (suspendida) menstruation, are described as perceived by poor Brazilian women in Northeast Brazil. Culturally prescribed methods to "regulate" these conditions and provoke menstrual bleeding are also described ...
Henshaw, S. K. (1991). "The Accessibility of Abortion Services in the United States" (PDF). Family Planning Perspectives. 23 (6): 246–263. CiteSeerX 10.1.1.360.6115. doi:10.2307/2135775. JSTOR 2135775.
Bloom, Marcy (25 February 2008). "Need Abortion, Will Travel". RH Reality Check. Archived from the original on 30 November 2008. Retrieved 15 June 2009.
Gomperts, Rebecca (2002). "Women on Waves: Where next for the abortion boat?". Reproductive Health Matters. 10 (19): 180–183.
Best, Alyssa (2005). "Abortion Rights along the Irish-English Border and the Liminality of Women's Experiences". Dialectical Anthropology. 29 (3–4): 423–437. doi:10.1007/s10624-005-3863-x. ISSN 0304-4092.
Lambert-Beatty, Carrie (2008). "Twelve miles: Boundaries of the new art/activism". Signs: Journal of Women in Culture and Society. 33 (2): 309–327.
Banister, Judith. (16 March 1999). Son Preference in Asia – Report of a Symposium Archived 16 February 2006 at the Wayback Machine.. Retrieved 12 January 2006.
Reaney, Patricia. "Selective abortion blamed for India's missing girls". Reuters. Archived from the original on 20 February 2006. Retrieved 3 December 2008.
Sudha, S.; Rajan, S. Irudaya (July 1999). "Female Demographic Disadvantage in India 1981–1991: Sex Selective Abortions and Female Infanticide". Development and Change. 30 (3): 585–618. doi:10.1111/1467-7660.00130. PMID 20162850. Archived from the original on 1 January 2003. Retrieved 3 December 2008.
"Sex Selection & Abortion: India". Library of Congress. 4 April 2011. Archived from the original on 27 September 2011. Retrieved 18 July 2011.
"China Bans Sex-selection Abortion" Archived 12 February 2006 at the Wayback Machine. (22 March 2002). Xinhua News Agency. Retrieved 12 January 2006.
Graham, Maureen J.; Larsen; Xu (June 1998). "Son Preference in Anhui Province, China". International Family Planning Perspectives. 24 (2): 72–77. doi:10.2307/2991929. Archived from the original on 21 October 2011.
"Preventing gender-biased sex selection" (PDF). UNFPA. Retrieved 1 November 2011.
"Prenatal sex selection" (PDF). PACE. Archived from the original (PDF) on 3 October 2011. Retrieved 17 November 2015.
Smith, G. Davidson (1998). "Single Issue Terrorism Commentary". Canadian Security Intelligence Service. Archived from the original on 15 October 2007. Retrieved 1 September 2011.
Wilson, M.; Lynxwiler, J. (1988). "Abortion clinic violence as terrorism". Studies in Conflict & Terrorism. 11 (4): 263–273. doi:10.1080/10576108808435717.
"The Death of Dr. Gunn". New York Times. 12 March 1993. Archived from the original on 10 November 2016.
"Incidence of Violence & Disruption Against Abortion Providers in the U.S. & Canada" (PDF). National Abortion Federation. 2009. Archived (PDF) from the original on 13 June 2010. Retrieved 9 February 2010.
Borger, Julian (3 February 1999). "The bomber under siege". The Guardian. London. Archived from the original on 22 February 2017.
Alesha E. Doan (2007). Opposition and Intimidation:The abortion wars and strategies of political harassment. University of Michigan. p. 2.
Spencer, James B. (1908). Sheep Husbandry in Canada. p. 114. OCLC 798508694.
"Beef cattle and Beef production: Management and Husbandry of Beef Cattle". Encyclopaedia of New Zealand. 1966. Archived from the original on 1 January 2009.
Myers, Brandon; Beckett, Jonathon (2001). "Pine needle abortion". Animal Health Care and Maintenance (PDF). Tucson, AZ: Arizona Cooperative Extension, University of Arizona. pp. 47–50. Archived from the original (PDF) on 28 July 2015. Retrieved 10 April 2013.
Kim, Ill-Hwa; Choi, Kyung-Chul; An, Beum-Soo; Choi, In-Gyu; Kim, Byung-Ki; Oh, Young-Kyoon; Jeung, Eui-Bae (2003). "Effect on abortion of feeding Korean pine needles to pregnant Korean native cows". Canadian Journal of Veterinary Research. Canadian Veterinary Medical Association. 67 (3): 194–197. PMC 227052. PMID 12889725.
Njaa, Bradley L., editor (2011). Kirkbride's Diagnosis of Abortion and Neonatal Loss in Animals. John Wiley & Sons. ISBN 9780470958520.
Overton, Rebecca (March 2003). "By a Hair" (PDF). Paint Horse Journal. Archived from the original (PDF) on 18 February 2013. Retrieved 19 December 2012.
Adams, Kye R.; Fetterplace, Lachlan C.; Davis, Andrew R.; Taylor, Matthew D.; Knott, Nathan A. (January 2018). "Sharks, rays and abortion: The prevalence of capture-induced parturition in elasmobranchs". Biological Conservation. 217: 11–27. doi:10.1016/j.biocon.2017.10.010.
"Herpesvirus in dog pups". petMD. Archived from the original on 9 November 2013. Retrieved 18 December 2012.
"Spaying Pregnant Females". Carol's Ferals. Archived from the original on 18 November 2012. Retrieved 17 December 2012.
Coates, Jennifer (7 May 2007). "Feline abortion: often an unnerving necessity". petMD. Archived from the original on 21 January 2012. Retrieved 18 December 2012.
Khuly, Patty (1 April 2011). "Feline abortion: often an unnerving necessity (Part 2)". petMD. Archived from the original on 18 November 2012. Retrieved 18 December 2012.
Schwagmeyer, P. L. (1979). "The Bruce Effect: An Evaluation of Male/Female Advantages". The American Naturalist. 114 (6): 932–938. doi:10.1086/283541. JSTOR 2460564.
McKinnon, Angus O.; Voss, James L. (1993). Equine Reproduction. Wiley-Blackwell. p. 563. ISBN 0-8121-1427-2. Archived from the original on 15 March 2015.
Berger, Joel W; Vuletić, L; Boberić, J; Milosavljević, A; Dilparić, S; Tomin, R; Naumović, P (5 May 1983). "Induced abortion and social factors in wild horses". Nature. 303 (5912): 59–61. doi:10.1038/303059a0. PMID 6682487.
Pluháček, Jan; Bartos, L (2000). "Male infanticide in captive plains zebra, Equus burchelli" (PDF). Animal Behaviour. 59 (4): 689–694. doi:10.1006/anbe.1999.1371. PMID 10792924. Archived from the original (PDF) on 18 July 2011.
Pluháček, Jan (2005). "Further evidence for male infanticide and feticide in captive plains zebra, Equus burchelli" (PDF). Folia Zoologica. 54 (3): 258–262. Archived (PDF) from the original on 22 February 2012.
Kirkpatrick, J. F.; Turner, J. W. (1991). "Changes in Herd Stallions among Feral Horse Bands and the Absence of Forced Copulation and Induced Abortion". Behavioral Ecology and Sociobiology. 29 (3): 217–219. doi:10.1007/BF00166404. JSTOR 4600608.
Agoramoorthy, G.; Mohnot, S. M.; Sommer, V.; Srivastava, A. (1988). "Abortions in free ranging Hanuman langurs (Presbytis entellus) – a male induced strategy?". Human Evolution. 3 (4): 297–308. doi:10.1007/BF02435859. |