7.1 Introduction
Transabdominal preperitoneal hernia repair (TAPP) was first published by M. Arregui in 1992. The procedure consists of several phases. The first one is not hernia specific. Establishment of pneumoperitoneum, introduction of the endoscope, exploratory laparoscopy and confirmation of the preoperative diagnosis. Second phase is the preperitoneal dissection in a clearly defined area (landing zone) in order to retract all hernia sacs (with or without content) and any prolapsing fatty tissue and facilitate the following step (phase 3). Placement of a large (15 × 10 cm or bigger) prosthetic mesh in the landing zone without any folds or wrinkles and taking measures to prevent early mesh dislocation (fixation, non-fixation). Phase 4 is the closure of the peritoneal opening and in phase 5 the CO2 is evacuated and working port incisions are closed.
7.2 Classification of Complications
In order to diminish avoidable complications to absolute minimum, there must be a systematic workout of all possible deviations of a normal course. There is no general classification of complications in hernia repair that would allow direct comparison of the surgical techniques, because the differences may be very intervention specific. Important is of course not only the incidence of a complication but its severity too.
A general severity classification is e.g. the Clavien-Dindo classification, which was revised and validated in 2004, ranges from class I, denoting minimal deviation from the normal postoperative course without the need for
pharmacological treatment or surgical, endoscopic or radiological intervention, to class V, indicating postoperative death.
Clavien-Dindo classification of postoperative complications:
I. Any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic and radiological interventions
II. Requiring pharmacological treatment with drugs other than such allowed for grade I complications
III. Requiring surgical, endoscopic or radiological intervention
IV. Life-threatening complication (including CNS complications) requiring IC/ICU management
V. Death of a patient
Despite the important value that this classification has, its use for TAPP repair of groin hernias is limited.
Thorough analysis of the whole procedure with all its obvious and hidden risks will be presented in order to help to prevent avoidable damage. It is difficult to avoid what is not well known. It is difficult to understand, if not well studied. It is easier to study the matter, if it is systematically described.
There is no generally accepted consensus on which deviation from “usual course” is or is not a complication. Therefore, the published results of complications may vary substantially.
Complications can be classified according to different aspects: according to consequences, to causality, to a specific phase of the procedure or the postoperative course.
7.2.1 In Relation to Consequences
Minor Haematoma, port-site infection, pneumonia, intestinal paralysis, early acute pain, urinary retention/ infection, seroma
Major Bladder injury, bowel injury, small bowel obstruction, big vessel injury, haemorrhage, mesh infection, trocar hernias, chronic pain, ischaemic orchitis and recurrence
7.2.2 In Relation to Causality
Nonspecific
Related to e.g. general anaesthesia, OR table, burns Laparoscopy
Access related, pneumoperitoneum related Dissection technique Vascular, nervous, organ injury, acute and
chronic pain Mesh
Infection, shrinkage, migration, recurrence, pain Fixation
Acute and chronic pain, recurrence Surgeon
Poor knowledge, poor orientation, poor performance
7.2.3 In Relation to Time
Intraoperative, early postoperative, late postoperative complications.
In his book “Chirurgie der Leistenhernie”, Bittner et al. (2006) published the incidence of intraoperative, early postoperative and late postoperative complications on a large collective of patients undergoing a TAPP repair of uncomplicated primary unilateral and bilateral hernias.
7.2.4 Intraoperative Complications
The numbers in brackets reflect all the hernia repairs performed including the complicated hernias too (recurrence, after preperitoneal repair open or laparoscopic, incarcerated or irreducible hernias, scrotal hernias and hernias after open prostatectomy or bladder surgery).
Some intraoperative complications may be specific for TAPP repair like visceral or bowel injuries, some may be addressed to general anaesthesia (circulatory complications, hypercarbia) and some result from incorrect dissection or misinterpretation of the local anatomy or too generous use of monopolar cautery.
7.2.5 Early Postoperative Complications
7.2.6 Late Postoperative Complications
The overall complication rate in this huge series is very low and reflects an immense experience of a dedicated team with a very high caseload (>1000/year). Under average conditions including teaching institutions, we have to assume that the true complication rate is much higher. The impact of experience as demonstrated by the same team shows how important is the standardisation of a new procedure, improving the operative skills, improving the anatomical knowledge and adhering strictly to the principals of minimal invasiveness in any TAPP hernia repair. In other reports from the early days of TAPP, one can recognise the same phenomenon of injuries to nervus cutaneus femoris lateralis due to imperfect knowledge of anatomy.
7.3 Access-Related Complications (Phase 1)
To perform a TAPP repair, it needs the insufflation of 2–4 lt. of CO2 to lift and expand the anterior abdominal wall to maintain the working space. This step carries a substantial risk of an injury to intra-abdominal structures.
Which is the safest and most effective method of establishing
pneumoperitoneum and obtaining access to the abdominal cavity?
The safest and most efficient method of access is still controversial [1–4]. There are four ways on how to obtain access to the abdominal cavity: (1) Open access (Hasson) (2) Veress needle to create pneumoperitoneum and trocar insertion without visual control (3) Direct trocar insertion (without previous pneumoperitoneum) (4) Visual entry with or without previous gas insufflation [7–12].
IEHS Guidelines 2011 [13]
Statements
Level 1A There is no definitive evidence that the open-entry technique for establishing pneumoperitoneum is superior or inferior to the other techniques currently available.
Level 1B In thin patients (BMI < 27), the direct trocar insertion is a safe alternative to the Veress needle technique.
Level 2C Establishing pneumoperitoneum to gain access to the abdominal
cavity represents a potential risk of parietal, intra-abdominal and retroperitoneal injury. Patients after previous laparotomy, obese patients and very thin patients are at a higher risk.
Level 3 Waggling of the Veress needle from side to side must be avoided, because this can enlarge a 1.6-mm puncture injury to an injury of up to 1 cm in viscera or blood vessels.
Level 4 The various Veress needle safety tests or checks provide insufficient information on the placement of the Veress needle. The initial gas pressure when starting insufflation is a reliable indicator of correct intraperitoneal placement of the Veress needle. Left upper quadrant (LUQ, Palmer’s) laparoscopic entry may be successful in patients with suspected or known periumbilical adhesions or history or presence of umbilical hernia or after three failed insufflation attempts at the umbilicus.
Recommendations
Grade A When establishing pneumoperitoneum to gain access to the abdominal cavity, extreme caution is required. Be aware of the risk of injury. The open access should be utilised as an alternative to the Veress needle technique, especially in patients after previous open abdominal surgery.
IEHS Update 2014 [14]
New statements—identical to previous except statement below.
Level 1B In thin patients (BMI < 27), the direct trocar insertion is a safe alternative to the Veress needle technique (stronger evidence).
New recommendations—identical to previous except recommendation below.
Grade C The direct trocar insertion (DTI) can be used in order to establish
pneumoperitoneum as a safe alternative to Veress needle, Hasson approach or optical trocar, if patient’s risk factors are considered and the surgeon is appropriately trained (new recommendation) [10].
Amongst general surgeons and gynaecologists, the most popular method is the Veress needle [1]. Although the open approach seems to be the safest, it does not eliminate the entire risk of injury [5, 6] (level 2C). When using open approach palpation through the peritoneal aperture, to exclude adhesions is mandatory before inserting a blunt cannula [6].
7.4 Trocar-Related Complications
Further development of trocar design, from cutting instrument (to diminish the necessary penetrating force) towards the dilating instrument, has reduced the complication rate of parietal (or intra-abdominal) haemorrhage and the risk of developing a trocar hernia.
According to IEHS Guidelines and its Update, cutting trocars should not be used anymore. The use of 10 mm trocars or larger may predispose to hernias, especially in the umbilical region or in the oblique abdominal wall (stronger evidence) (level 2B). Therefore, fascial defects of 10 mm or bigger should be closed (stronger evidence) (grade B).
Concerning the closure of trocar wounds ≥10 mm, I believe in closing the peritoneal layer too. The reason is the obvious difference in trocar hernia incidence in TAPP and TEP repair.
7.5 Dissection-Related Complications (Phase 2)
Poor knowledge of anatomy, not recognising the structures, wrong use of energy sources, impatience, lack of skills or too difficult dissection (e.g. after previous surgery) [16, 17] may lead to injury of big vessels, nerves, bowel, bladder, spermatic cord or spermatic vessels.
Vessels “at risk”
Inferior epigastric, iliac and spermatic can be injured by the trocar, during the dissection or by fixing device.
Nerves “at risk”(0.3 %) During the dissection of the landing zone, the genital branch of the genitofemoral nerve, the lateral femoral cutaneous and the femoral nerve can be directly sectioned, damaged by coagulation or fixation device (see fixation-related complications below). The latter can injure even the ilioinguinal or iliohypogastric nerve depending on penetration depth of the device.
Major nerve injuries after laparoscopic hernioplasty have been reported, but the
risk of this complication appears to be extremely low. In the early days of TAPP, these injuries reflected the lack of knowledge of the local anatomy or indelicate dissection.
The “triangle of pain” (lateral of spermatic vessels and below the iliopubic tract) as an area of nerves at risk had to be enlarged to about 1.5–2 cm above the iliopubic tract thanks to the brilliant anatomic study of Reinpold.
The incidence of sensory changes after a TAPP repair seems to be ten times lower than after an open repair (p < 0.001) [15].
7.6 Visceral Injuries (Bladder, Intestine) 0.1 %
Keywords
Veress needle, First and second trocar, Lack of overview, Delayed thermic lesions, Previous abdominal surgery, Lack of experience
Entering the abdominal cavity (with or without previous surgery) and during the preperitoneal dissection, there is an instant risk of bowel or bladder injury. Half of the big vessel injuries were reported to be caused by the second trocar! That means under visual control! Lack of force coordination or even worse lack of concentration may lead easily to a major complication. It is a great advantage of TAPP when compared to TEP that the procedure starts with existing working space. To move the long instruments in this space without endangering the fragile structures within is a must, but it is an ability developed after many laparoscopic operations. Even in easy repairs, the concentration must be maintained from the insertion of Veress needle till the last skin suture.
The chance to “look back” (from preperitoneal space to intraperitoneal space) during the dissection of the landing zone, especially in triangle of doom and triangle of pain, lets the operator control the bowel behind. Steeper Trendelenburg position may bring the bowel in safe distance.
Despite the fact that a urinary catheter is in general not recommended, in some complicated cases it may be of great value. Dissection after open prostatectomy or after previous prosthetic preperitoneal repair may become quite difficult. Not only the empty bladder, but the possibility of retrograde instillation (e.g. methylene blue) may be advantageous to detect and control eventual bladder injury.
In case of necessary adhesiolysis, any suspicion of serosal lesion must be scrutinised. Oversewn serosa tear is more secure than a missed one.
The adhesiolysis of hernia content is not advisable. The hernia sac (e.g. in sliding hernias) is mobilised in toto with the content during the preperitoneal
dissection.
The most dangerous condition is the unrecognised enterotomy or delayed enterotomy. The latter mostly caused by inappropriate use of monopolar cautery with consecutive tissue necrosis and delayed onset of postoperative peritonitis. Therefore, even after an easy procedure, stay alert to any unusual symptom after a laparoscopic hernia repair.
7.7 Seroma, Haematoma 0.29–4 %
Keywords
Pseudo-recurrence, Hernia size, Hernia type, Rare reoperation 0.46 %, Aspiration seldom necessary [20].
The bigger the hernia sac is, the bigger the chance of development of a seroma formation.
In large indirect sacs, the recommended complete retraction may lead to higher incidence of haematomas and may compromise the blood supply to the testicle. The transection of the indirect sac and leaving the distal portion open shows higher incidence of seromas and may lead in later course to development of a pseudo-hydrocoele. Fixing the distal portion to the abdominal wall lateral to epigastric vessels seems to help to avoid the occurrence of seromas [26].
In larger direct hernias (M2-3), the incidence of seromas can be significantly reduced by inversion of transversalis fascia and fixation to Cooper’s ligament with tacks [18, 19] or using an Endoloop [24, 25]. This step diminishes the dead space for seroma formation but additionally obliterates the potential of mesh dislocation into previous hernia space.
Inversion of the transversalis fascia is associated with a statistically lower incidence of postoperative seroma, without increasing postoperative pain despite the use of one or two additional tacks [19].
Update IEHS
New statements—identical to previous except statement below.
Level 4 Alternatively to fixation of the extended fascia transversalis to Copper’s ligament, the direct inguinal hernia defect can be closed by a pre-tied suture loop. (new statement).
New recommendations—identical to previous except recommendation below.
Grade D As an alternative, the primary closure of direct inguinal hernia defects with a pre-tied suture loop can be used (new recommendation).
New Literature [24]
Prospective study, 250 patients, , 94 direct hernias, 76 were M2 or M3, were treated with ligation of the everted direct sac with PDS Endoloop [24]. 1.3 % residual seroma at 3 months, no chronic groin pain and no hernia recurrence after a median follow-up of 18 months.
Conclusion: The primary closure of direct inguinal hernia defects with a pre-tied suture loop during endoscopic TEP repair is safe, efficient and very reliable for the prevention of postoperative seroma formation, without increasing the risk of developing chronic groin pain or hernia recurrence.
7.8 Urinary Retention: POUR 0.42–3.1 %
POUR is probably of multifactorial origin. There is no general indication for preoperative catheterisation, and there are no clear predictive factors for postoperative retention. It is advisable that the patient empties the bladder before surgery. Full urinary bladder during a TAPP repair increases the risk of a bladder injury and can make the dissection even more difficult. In patients with expected technical difficulties (after previous abdominal, prostatic or bladder surgery) or extended operating time (bilateral scrotal, in learning curve), preoperative catheterisation should be considered.
Postoperative urinary retention is more frequent in endoscopic repairs (under general anaesthesia – GA) then in open hernia repairs under local anaestesia, possibly due to inhibitory effect of GA on bladder function [27].
Urinary retention may significantly prolong the hospital stay. With consequent approach towards possible POUR—preoperative emptying, restrictive fluid management in the early postoperative phase, early mobilisation and refrain from opioids—the incidence of retention can be as low as 0.5 % [28].
7.9 Testicular Problems 0.15 %
7.9.1 Testicular Atrophy (0.04–0.09 %)
Keywords
Testicular pain, Hydrocoele, Ischemic orchitis, Venous congestion, Nerve irritations, Leaving the indirect sack in situ
7.9.2 How to Avoid Testicular Problems?
The early postoperative tenderness of testis is often related to dissectional trauma or just irritation of genital branch of the genitofemoral nerve. Gentle dissection in correct plane with preservation of spermatic fascia protects the nerve; prudent use of monopolar cautery is most probably safer than incomplete haemostasis. Separating peritoneum from spermatic cord and vessels (parietalisation) seems to be easier if these structures were lifted by the nondominant instrument and the peritoneum pulled down by the dominant instrument. However, this is absolutely not necessary; there is always a way to grasp adjacent tissue to facilitate this step and avoid any possible injury to spermatic structures. The “no touch technique” is our policy.
Another possible reason for testicular pain was the lateral slit in mesh in order to pass the lower tail under the cord and vessels and close it again with the upper tail (analog Lichtenstein). The idea of slitting the mesh was to prevent the dislocation of the low lateral corner above the triangle of pain. The solution to this is a generous parietalisation and a non-penetrating fixation with fibrin sealant or cyanoacrylate glue. Late transection of spermatic duct caused by shrinkage of a slit mesh was published. The IEHS Guidelines do not recommend slitting the mesh (see below).
7.10 Mesh-Related Complications
7.10.1 Mesh Shrinkage
7.10.1.1 Factor Mesh Material vs. Mesh Construction
Not only variable polymers (polypropylene PP, polyester PE, polytetrafluoroethylene PTFE or polyvinylidene fluoride PVDF) but the mesh product itself induces different behaviour of the recipient after the mesh is implanted. Mesh size, its strength, total foreign body weight, porosity (the most important property), shrinkage rate, bridging and flexural rigidity may influence the final outcome.
The microporous meshes (most often heavyweight meshes) show an excessive shrinkage rate (compression by the scar tissue formation as a consequence of a strong inflammatory foreign body reaction). The most modern mesh products are macroporous. The difference between the macroporous lightweight meshes and the microporous heavyweight meshes in form of less local discomfort, chronic pain or a foreign body feeling could not be demonstrated in any study of TAPP or TEP repair.
7.10.2 Mesh Infections
Mesh infections in TAPP are nearly inexistent, but anecdotic reports were published [29–32].
7.10.3 Recurrence TAPP 0.27–3.7 %
7.10.3.1 Reasons for Recurrence
Technique
Lack of experience
Insufficient extent of dissection
Missed hernia
Preperitoneal lipoma
Suboptimal mesh placement
Inappropriate retention/fixation
Mesh lifted by haematoma
Inferior lateral mesh edge lifted at closure
Material
Microporous mesh
Heavyweight mesh/excessive shrinkage
Size to small
Insufficient overlap in relation to shrinkage
Mesh slit
Mesh protrusion
Risk Factors
Collagen disease
Smoking
Obesity
Malnutrition
Diabetes Type ll
Chronic lung disease
Coagulopathy
Steroids
Radiotherapy, chemotherapy
Jaundice
Male gender
Anaemia
The most important causes of recurrence after a TAPP repair are avoidable. Small mesh, insufficient extent of dissection, incorrect mesh placement, slotted mesh, missed lipoma, sliding retroperitoneal fat, insufficient fixation, non-fixation in a wrong indication, all of them being a technical underestimation of a true problem rather than lack of knowledge [31, 36].
The recommended mesh size for TAPP repair is 15 × 10 cm or larger [14,
33–35]. Smaller meshes are the most important cause of hernia recurrence today. Mesh slit should have had prevented possible mesh dislocation, instead of
that it increased the recurrence rate [33]. Leibl demonstrates that both small mesh size and the slit in mesh increased the risk for recurrence. Heikinnen [38] changes his policy in TAPP repair from Surgipro 6 × 10 cm to Prolene 10 × 14 cm and reduces his recurrence rate from 28 to 0 %. Felix [37] found in six patients with chronic testicular pain four patients with a keyholed mesh. It might be speculated whether the slit predisposed the nerve to injury or chronic irritation from the mesh.
Phase 1 Slitted mesh, 13 × 8 cm
Cause of recurrence Mesh too small
Recurrence rate 2.8 % slit region insufficient
Phase 2 Nonslotted, 15 × 10 cm
Cause of recurrence Mesh dislocation
Recurrence rate 0.36 %
From Leibl et al. [33]
7.10.4 Pseudo-recurrence
Seroma in the early postoperative course maybe wrongly understood as a recurrence. Ultrasound helps to clarify. Overlooked lipoma in inguinal or femoral canal may present as a recurrence too and will most probably lead to a revision or removal through anterior approach after the nature of the local swelling was confirmed by MRI.
Protrusion of a lightweight mesh into a large direct defect is rare, but a true
recurrence, despite the correct size and placement of the prosthetic material. In such situation, meshes with higher flexural rigidity are recommended.
7.10.5 Mesh Displacement, Erosion, Migration
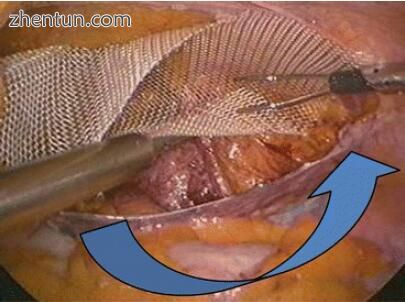
The most common reason for a mesh dislocation is its insufficient size and imperfect placement. The lower margin of the “landing zone” has to allow placing the mesh over psoas muscle without lifting up the low lateral mesh corner when closing the peritoneum. Penetrating fixation (staples, tackers, sutures, etc.) do not compensate for “incorrect” placement. Soft fixation (sealants and glues) may prevent an early movement and decrease the recurrence rate.
Excessive shrinkage of some meshes may also contribute to mesh displacement or to “meshoma” formation.
The few but true reports of late migration and erosion into adjacent organs stress again the importance of strict adherence to the rules of TAPP repair. These unusual complications seem to be the consequence of technical errors [39–46].
7.11 Fixation-Related Complications
7.11.1 Haemorrhage, Injury to Nerves, Acute Pain, Chronic Pain, Recurrence
Knowledge of the local anatomy should eliminate the risk of injury of big- and medium-sized vessels during dissection or mesh fixation. Penetrating fixation
seemed in the past to be necessary to prevent mesh dislocation. Over time, we have learned that mesh retention rather than fixation is only a temporary need, until host tissue ingrowth will take place. The macroporosity of the implant would support the ingrowth without pronounced shrinkage. This fact led to the introduction of fibrin sealant and glue fixation [76–80, 83–86].
Penetrating fixation does not compensate if the mesh is too small. Temptation to fix the mesh with tackers, staples or sutures in triangle of doom or triangle of pain can lead to disasters. For example, in order to prevent the dislocation of “the critical corner” causing a long-lasting neuropathy of genitofemoral nerve.
A spiral tack injuring genitofemoral nerve (Courtesy of Jorge Cervantes, Mexico)

A spiral tack injuring genitofemoral nerve (Courtesy of Jorge Cervantes, Mexico)
Tack in pulmonary artery after TEP (Courtesy of Jorge Cervantes, Mexico)
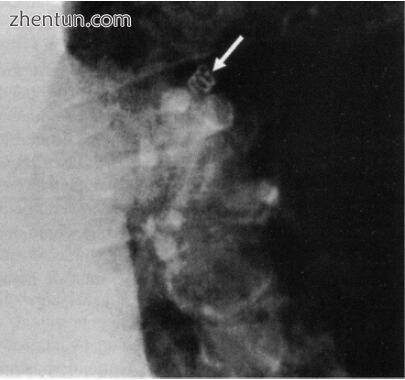
Tack in pulmonary artery after TEP (Courtesy of Jorge Cervantes, Mexico)
There is a clear trend in TAPP and TEP repair towards soft fixation or non-fixation [47–52].
Lovisetto [53] compared in a RCT staples vs. fibrin glue mesh fixation in TAPP repair. It shows a lower incidence of postoperative neuralgia and an earlier resumption of physical and social activities in patients with soft fixation.
Kapiris [22] publishes excellent recurrence rate of 0.16 % in a large cohort of TAPP repairs with 15 × 10 cm meshes and no fixation in a long follow-up.
Akolekar [54] shows a rise of recurrence rate in TEP repair with non-fixed meshes since the introduction of lightweight meshes. All above teams are experts in their discipline, so the simple technical errors are less probable.
There is probably more than just the mesh size and its rigidity. The size of the defect both in direct as well as indirect hernias shows even in open repairs the higher risk for recurrence.
7.12 Conversion 0.0–6.2 %
Conversions in TAPP are very rare. Hostile abdomen should be ruled out preoperatively as a relative contraindication for TAPP due to inadequate risk of bowel injury. However, even after uncomplicated appendectomy, cholecystectomy or C-section, one can encounter extensive omento-parietal adhesions. Depending on surgeon’s experience and the extent of adhesions, it is
wise to convert early enough before damage is done. Unforced conversion to open anterior repair can lead to better results; forced conversion as an “ultima ratio” after serious injury lead to laparotomy and higher complications rate. Lack of overview can lead to missed enterotomy with all its consequences.
Prudent patient selection, proper teaching and enough self-criticism are the best counsellors.
7.13 Closure-Related Complications
7.13.1 Small Bowel Obstruction
IEHS Guidelines on Peritoneal Closure Statements
Level 3 Incomplete peritoneal closure or its breakdown in endoscopic, preperitoneal hernia repair increases the risk of bowel obstruction.
Level 3 TAPP procedure presents a higher statistical risk of small bowel obstruction than TEP.
Level 5 The most appropriate peritoneal closure is achieved by running absorbable suture.
Level 5 Running suture seems to cause less pain compared with clip/tack closure.
Level 5 The closure of entrance of indirect sacs may reduce the risk of internal hernia with consecutive incarceration, strangulation or small bowel obstruction.
Recommendations
Grade C A thorough closure of peritoneal incision or peritoneal tears should be done.
Grade D The peritoneal closure can be accomplished by a running suture.
Bowel obstruction can develop due to adhesions between omentum or epiploic appendices and suture line, between the mesh and the intestines, e.g. caused by inadequate closure of a peritoneal lesion [55–57]. The peritoneal opening must be thoroughly closed to prevent contact of viscera with the prosthetic mesh material and to reduce the risk of bowel obstruction. This closure can be achieved with staples, tackers, running suture or glue. These last two methods are more time-consuming but less painful [58, 59] (see Chap. 9). Rare cases of bowel obstruction in port-site hernias also have been described, especially after TAPP. Several anecdotic reports on small bowel obstruction both in TAPP [60]
and TEP repairs have been published [61, 62]. The data from Swedish National Inguinal Hernia Register show higher incidence of late postoperative bowel obstruction after TAPP than after TEP [55].
IEHS Guidelines Update on Peritoneal Closure New statements—identical to previous.
New recommendations—identical to previous except the statement below.
Grade B A thorough closure of peritoneal incision or of bigger peritoneal tears should be achieved (stronger evidence).
The previous recommendation on peritoneal closure already connoted verbally the importance of the task, although assigned to Grade C. To emphasise the fact, this recommendation was upgraded to Grade B.
Ross et al. [63] reported that the postoperative activity limitation at 2 weeks was significantly better in the suture group when compared to the stapled group (p = 0.005). Additionally, sutured PF closure had less early postoperative pain when compared to the tacker group (p = 0.038). He concluded: Following TAPP IHR, suture closure of the peritoneal flaps significantly improve 2-week postoperative movement limitation compared to stapled and tacked peritoneal closure.
Köhler et al. [64] raise attention to a new cause of small bowel obstruction owing to strained adhesions and ingrowth between a small bowel segment and a polyglyconate unidirectional self-anchoring barbed suture device (V-lock) (this has to be cut short at the end of a running suture).
Similar report was presented by Fitzgerald et al. [65]—small bowel obstruction due to displaced spiral tack.
7.13.2 Port-Site Hernias 0–6.2 %
Port-site hernia is a late postoperative complication predominantly reported in TAPP repair. Although, according to general opinion, only 10 mm and bigger trocar site defects should be closed [14, 35, 66], development of incisional hernia with consequences was described even with 3–5 mm trocars [67, 68].
IEHS Guidelines Update 2014 raises the questions: What kind of trocars should be used? Is there any relation between the trocar type and risk of injury and/or trocar hernias?
New statement—identical to previous except statement below.
Level 2B The use of 10-mm trocars or larger may predispose to hernias, especially in the umbilical region or in the oblique abdominal wall (stronger evidence).
New recommendation—identical to previous except recommendation below.
Grade B Fascial defects of 10 mm or bigger should be closed (stronger evidence). Upgraded.
The design of dilating, instead of cutting trocars, contributed significantly to decrease the risk of port-site bleeding and development of port-site hernias [59, 69–72]. Bittner et al. found significant differences in incidence of trocar-related parietal haemorrhage (cutting trocar 1.76 vs. 0.056 % conical trocar, p > 0.0001) and incidence of trocar hernias (cutting trocar 1.27 vs. 0.037 % conical trocar, p > 0.0001)
7.14 Chronic Pain 0.03–2.2 %
The aetiology of chronic pain (CP) is still not exactly known; it seems to be of multifactorial origin (surgeon-related, mesh-related and patient-related causes). It is often associated with incorrect dissection, with inadequate use of monopolar cautery; with penetrating and/or permanent fixation, with anatomically incorrect fixation, with patient’s individual inflammatory response to local dissection, with the implant or with pre-existent pain syndrome. Chronic postoperative pain following TAPP and TEP is more prevalent than recurrence [73]. Preoperative pain, repair for recurrent groin hernias (following anterior repair) and younger age at surgery seem to predict development of chronic postoperative pain. Identification of “patients at risk” may improve the choice of surgical procedure and reduce morbidity and cost [74, 75].
The randomised study by Singh et al. [81] showed that preoperative pain, younger age, open surgery and 7-day postoperative pain were independent risk factors for chronic pain.
Chronic pain syndrome is seldom seen in endoscopic hernia repair [82]. According to Aasvang et al. [83], the overall incidence of chronic pain after open groin hernia repair is 18 % (range, 0–75.5 %) and 6 % after endoscopic repair (range, 1–16 %; p=0.01) The risk of acute and chronic pain is lower after endoscopic groin hernia repair compared with open surgery with or without mesh. The risk of sensory disturbances of the groin is lower after endoscopic
groin hernia repair compared with open surgery with or without mesh [79]. No consensus guidelines exist for the management of postoperative chronic
pain yet [73, 76], despite many scientific papers about this troublesome condition during the last 10 years. There is a need for guidelines regarding management of chronic pain.
In between, it is more important to try to avoid anything that could lead to CP. Anatomically correct and gentle dissection, wise use of cautery, macroporous meshes, noninvasive fixation using glues or sealants or no fixation in P, L1-2/ M1-2 hernias, no tackers when closing peritoneum, correct indication for surgery and proper choice of patients, considering their individual factors seem to be the right way to go.
7.15 Infertility, Dysejaculation?
Although animal studies have suggested a strong correlation between mesh inguinal hernia repairs and structural damage to elements of the spermatic cord and testicle [89], this has not translated into a clinically significant infertility rate after open or laparoscopic inguinal hernia repair [14] (Fitzgibbons in Update of IEHS Guidelines), [87, 88].
New Statement
Level 2B Inguinal hernia repair with mesh is not associated with an increased risk of, or clinically important risk for, male infertility.
New Recommendation
Grade B Groin hernia repair using mesh techniques may continue to be performed without major concern about the risk for male infertility.
Peeters [90] reported a possible adverse effect on sperm motility 1 year after TEP repair with lightweight meshes, but could not confirm it at 3 years follow-up [91].
In a Danish study including men undergoing laparoscopic inguinal hernia repair who were registered in the Danish Hernia Database, dysejaculation occurred in 3.1 % [92].
7.16 Management of Possible Problems
7.16.1 Pneumoperitoneum
If using Veress needle, lift the skin with two graspers/forceps. After 3 nonsuccessful punctures periumbilically, use another localisation (Palmer’s point, subcostal left) or open access (Hasson). When the abdomen does not grow despite of proper gas flow, think of having punctured a hollow organ (stomach, bladder, intestine). Search for a possible injury, after introducing the endoscope, at the place where you punctured (posterior wall, vessels).
7.16.2 Trocar Injury
Immediate resolution recommended.
Serosa lesions of bowel loop: it is, probably, preferable to suture after placement of working ports.
Small bowel full-thickness lesion without massive spillage—intra-abdominal suture is possible. In doubt, do not expect typical fluid coming out of the lesion because of the intra-abdominal pressure. If not enough skilled, exteriorise the loop and repair outside. In case of no gross contamination, cover with omentum major and proceed with the rest of surgery.
Large bowel lesions must be thoroughly sutured. In case of obvious contamination, the surgeon shall proceed to a change of strategy: either open repair or postpone mesh implantation until one is sure the suture was successful and there’s no active peritonitis going on.
Parietal bleeding: Haemostasis with compression, peanuts soaked with diluted adrenalin, bipolar coagulation or suture. Control the result at reduced IAP. Remember that cutting trocars belong to museum.
Injury of big vessels: laparotomy.
Conversion: preferably unforced decision before too late. Repair what you can repair; otherwise call for a specialist.
7.16.3 Dissectional Injuries
In all patients, especially in those under any kind of anticoagulation (even Aspirin cardio) or with coagulopathy, consequent haemostasis is required. Do not rely on nature or drains.
Epigastric vessels: Prefer clips rather than just coagulation, transfascial sutures below and above the lesion. The closer to the iliac vessels, the more difficult it may get to repair the damage.
Iliac vessels: Be aware of the anatomy; stay away, at respectful controllable distance. Behave as requested in triangle of doom and in triangle of pain.
Corona mortis, suprapubic vessels, vessels around the femoral canal: These vessels have to be left where they are. Remember anatomy. Keeping the operative field dry guarantees better orientation and recognition of the important structures.
Bladder injury: If in doubt, retrograde instillation of diluted methylene blue, suture and Foley catheter. In case of previous surgery in preperitoneal space (TAPP, TEP, prostatectomy, section alta, etc.), anticipate problems and catheterise preoperatively.
7.16.4 Postoperative Problems
Acute postoperative pain: Most patients have after TAPP repair very moderate or even low level of pain in the first 12 h. Unexpected and inadequate acute pain asks for explanation. Early re-laparoscopy rules out doubts; explant tackers or staples if used.
Peritonitis: Early revision laparoscopy recommended.
Ileus: Early re-laparoscopy Infection: Drainage, antibiotics, mesh removal Seroma: Inform patients preoperatively, wait, aspirate after 1–3 months and operate after 6–12 months if still symptomatic.
Chronic pain: Wait, take care of pain, accompany the patient; most get better and will not need any treatment in the future. Contact a local pain centre; rule out other possible pain causes. Concern involving specialists, local and peripheral infiltrations. Do not try to reoperate before 6–12 months, unless you have found a clear reason to do so.
Recurrence: In case of a rare recurrence after a TAPP repair, use the opposite (open) approach if not already has been used previously (recurrence after Lichtenstein/mesh-free tissue repair and TAPP/TEP). Try to find out the true reason for recurrence (e.g. small mesh, no fixation, lightweight mesh in a big direct hernia) and consider your experience before you decide to proceed.
7.16.5 How to Prevent Complications?
Even the most simple primary groin hernia deserves full attention. Profound knowledge of anatomy of both anterior and posterior approach to groin hernia repair is indispensable. Consequent haemostasis is the key. Good overview and correct anatomical orientation prevent the majority of possible complications.
“TAPP repair” is a very well-standardised procedure. Although the average operation time is a kind of a mirror of operator’s experience, the surgery takes as long as it is necessary to accomplish the so-called perfect repair. Indirect hernia, e.g. takes longer than the direct one. Do not forget what the objective of a hernia
repair is: Patient’s satisfaction!
It is the surgeon’s state of mind that creates higher demands in order to achieve the best possible results.
Obey the rules: pneumoperitoneum, dilating trocar, under direct vision, consequent haemostasis, cautious use of cautery, cautious adhesiolysis, convert before too late, stay away of big vessels, respect nerves. Noninvasive fixation if any, adequate mesh size. Complete closure of peritoneal gap and closure of trocar incision (Table 7.1).
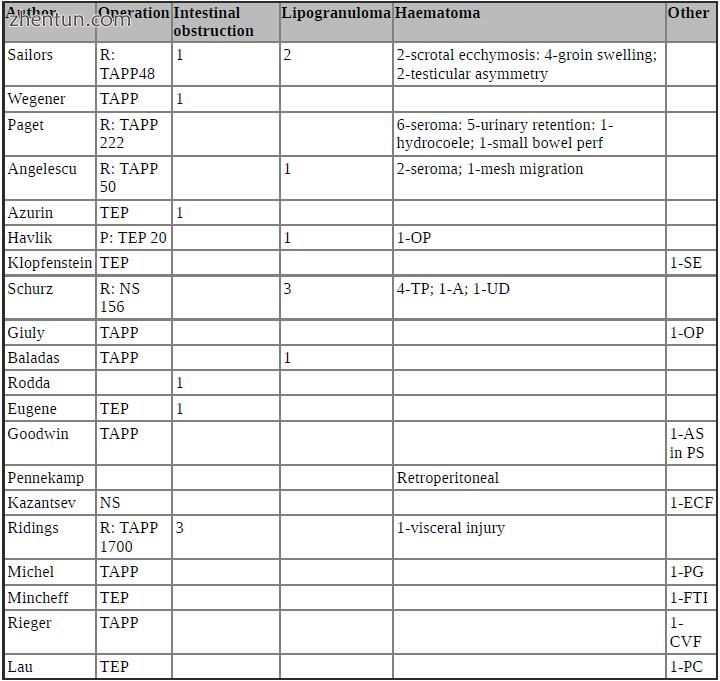
Table 7.1 Reports of complications after laparoscopic hernia repair
NS not stated, SE subcutaneous emphysema, PS port site, OP osteitis pubis, PC preperitoneal collection, FTI focal testicular infarction, CVF colovesical fistula, ECF enterocutaneous fistula, AS appendicular strangulation, PG pyoderma gangrenosum, UD undefined, A abdominal, TP transperitoneal, R retrospective study, P prospective study
7.17 Summary
The overall complication rate in laparo-endoscopic hernia repair is low. True incidence of complications is in fact unknown, because of underreporting. The individual surgeon determines the outcome far more than the procedure he chooses to use.
Complications are avoidable by awareness, knowledge, proper teaching and mentoring, disciplined dissection, perfection of skills, attention to details, wise selection of patients and experience.
How to avoid a complication?
Prevent it!
How to prevent a complication?
Follow the correct path, anticipate possible complications and act accordingly (start re-reading the above thoughts).
参考:Complications in Laparoscopic Surgery A Guide to Prevention and Management |