3.1 Introduction
Gastro-oesophageal reflux disease (GERD) is one of the most frequent benign disorders of the upper gastrointestinal tract and has a high prevalence in western countries.
GERD is the failure of the anti-reflux barrier, allowing abnormal reflux of gastric contents into the oesophagus, which causes different symptoms and complications.
It is a mechanical disorder, caused by a defective lower oesophageal sphincter (LES). The European Association of Endoscopic Surgery (EAES) [1] has evaluated 18,490 articles to establish current guidelines in the consensus development conference in 2013. According to the report of this conference, surgery is a successful therapeutic option, in well-selected patients, instead of long-term medical treatment that is purely symptomatic.
The goal of the surgical treatment for GERD is to restore this defective zone and create a new barrier to prevent gastro-oesophageal reflux.
The aim is to decrease the reflux symptoms, curing the oesophagitis and improving quality of life by the creation of a new anatomical high-pressure zone.
This must be achieved without dysphagia.
The main anti-reflux surgical procedures are based on the wrapping posteriorly of the gastric fundus, total or partial, around the oesophagus, obtaining a new valve able to contrast the reflux when the stomach is full and to adequately relax during swallowing, preventing postoperative dysphagia.
Rudolph Nissen [2] was the first to pioneer anti-reflux surgery in 1956. Although his first approach, 360° fundoplication procedure, improved reflux symptoms, some patients were troubled by dysphagia, bloating and the inability to belch “gas-bloat syndrome.” To avoid these side effects, in 1963 André Toupet [3, 4] created a posterior partial (270°) fundoplication, and Belsey [5] and Hill [6] would follow in 1967, with their approaches aimed at restoring the normal physiology of the lower oesophageal sphincter (LES). Subsequently, Mario Rossetti [7] proposed in 1977 a revision that included a modified total fundoplication with minimal dissection of the cardia and no division of the short gastric vessels (SGVs). DeMeester [8] published his “floppy Nissen modification” and successful outcomes in 1986. It concerned a very short 360° fundoplication in a tension-free manner by dividing the short gastric vessels.
More than three decades after the original fundoplication technique which was described by Rudolf Nissen, the first laparoscopic anti-reflux interventions that are based on the creation of a new valve with gastric fundus around the oesophagus, able to contrast the reflux, was described by Bernard Dallemagne in 1991 [9–11].
Since the first laparoscopic anti-reflux procedures, surgical techniques have gradually become standardised and have ended up being the “gold standard” for the treatment of gastro-oesophageal reflux.
Nowadays, laparoscopic anti-reflux surgery is the treatment of choice for patients with recurrent symptoms after suspension of the medication, poor responders to PPI and those not compliant to a long and expensive medical therapy (especially young patients).
Today all types of fundoplication can be carried out in good conditions for well-selected patients, in accordance with well-defined rules. However, surgery is burdened by some complications, side effects and non-negligible reintervention rates [12].
3.2 Complications in GERD
3.2.1 Generality
Surgical complications of laparoscopic techniques for GERD are generally rare
and due to non-compliance with well-codified rules. Certainly, lack of experience of the operator is one of the main risk factors for complications [13]. At the beginning, during the first learning phase, the main difficulty resided in the dissection of the oesophageal hiatus, particularly of the posterior surface of the oesophagus, where the appearance of a certain number of complications, even intra-operative perforations were common.
Progressively, better standardisation and understanding of the laparoscopic view and management of the hiatal region, including dissection in contact with the pillars of the diaphragm, the distance to the oesophagus, the development of instruments for laparoscopic surgery, as well as the appearance of teams with experience have allowed to reproduce techniques, with fewer complications, and more effectively.
Complication rate is often higher at the beginning of the experience, but, in general, it will stabilise after 50 procedures performed by a team and after 20 individual operations per surgeon [14].
Complications of laparoscopic treatment of GERD are the incidents that occur during intervention or the ones that appear during the postoperative course. They are related to the technique, to the experience, to the instrumentation and terrain, etc. and can be of two kinds:
Intra-operative complications (minor or serious)
Postoperative complications (failures) (immediate or delayed)
3.2.2 Intra-operative Complications
Intra-operative complications of laparoscopic anti-reflux procedures are essentially traumatic and involve mainly the oesophagus, stomach, pleura and vessels.
As shown in Table 3.1, the publication of Champault [15] related to a multicentre study by the SFCL (French Society of Laparoscopic Surgery) in 1994, the morbidity rate was 5 % with 940 cases of anti-reflux surgery, and in the series of Dallemagne [16] in 1995, with 2149 cases, the complication rate was addressed 1.6 %.
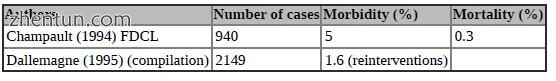
Table 3.1 Complication rate of the multicentre study of the SFCL (French Society of Laparoscopic Surgery) in 1994 [15] and of the series of Dallemagne [16] in 1995
3.2.3 Complications/Multicentre Series
Another most recent multicentre study of 7531 patients operated on between 2005 and 2009 shows a 3.8 % morbidity and 0.19 % mortality [17].
Intra-operative complications can be classified into three main groups:
Bleeding-haemorrhage
Perforation (oesophagus, stomach)
Other (pneumothorax-capnothorax, pneumomediastinum-capnomediastinum, laceration, injury or ischaemia in surrounding tissues or organs – liver, stomach, spleen, etc.
3.2.3.1 Haemorrhage
Haemorrhagic complications are rarely reported in literature. The overall rate of bleeding is low and usually without vital impact (rare cause of conversion and of transfusions).
Sometimes the type of intervention favours the bleeding. Dissection and section of the short gastric vessels during Nissen’s operation may cause injury of the spleen or short vessels (Video 3.1). Nissen-Rossetti, Toupet or Hill’s techniques do not seem to cause this type of injury. One of the major bleeding complications is the serious injury of the spleen; this, fortunately, is exceptional in laparoscopic surgery, while, on the contrary, it was quite common during open surgery [15].
A wound of the vena cava inferior or aorta can cause a very severe haemorrhagic accident; this may occur during the dissection of mediastinal oesophagus, during suturing of the diaphragmatic crus or when attaching a prosthesis on the hiatal defect. Be careful.
Otherwise, no significant bleeding from wounds in relatively small vessels or the liver injury by the retractor can often occur without serious consequences and are, often, stopped with a simple coagulation or ligation (Video 3.2).
Contrary to this, recklessly cutting a large left hepatic artery without effective haemostasis can be a cause of serious bleeding (Video 3.3). In the case of a large artery, effective control with ligatures, clips or LigaSure or ultrasonic dissection should be absolutely made before the section.
Video 3.1: Haemorrhage short gastric vessels
Video 3.2: Bleeding from relatively small vessels
Video 3.3: Serious haemorrhage during inattentive dissection of the lesser curvature
3.2.3.2 Digestive Perforations
Digestive Intra-operative complications are primarily represented by perforation of hollow organs (oesophagus and stomach). These complications were rarely mentioned in open series and seem to be rather specific of laparoscopy.
The series of the first years, in the beginning of laparoscopic GERD treatment, some cases of gastrointestinal perforation were published. With increasing experience and because of other reasons, these serious complications are rarely described in the most recent series.
In a survey by the French Association of Surgery, from 1999 [18] which includes 2424 cases from 21 centres, 25 gastrointestinal perforations were reported; 13 are perforations of the oesophagus and 12 of the stomach, with the need for 5 major surgeries and 2 deaths. Champault [15] has reported eight perforations in the research done by the FDCL, in 1994. Hinder [19] has reported 20 cases in 2453 patients. These perforations are estimated to be around 1 % and are quite serious as they are responsible for the majority of deaths reported in those series.
There is a classic mechanism to cause these wounds of the oesophagus and stomach:
Peri-oesophagitis with the cardia fixed in the lower mediastinum
The brachy-oesophagus;
Reoperations
Bad dissection plane with forceful passing behind the oesophagus
Perforation during passage of the tube (Faucher or other)
Electrical lesions of the oesophagus
Aggressive use of the instruments
Perforation by dropping stitches
Large hiatal hernia
Obesity
3.2.3.3 Oesophageal Perforation
Oesophageal perforation is the most important complication of anti-reflux surgery. It represents 0–2 % of cases depending on the series, occurring mainly during the phase of retro-esophageal hiatal dissection region. The consequence varies and can be detected early or late. If it is discovered during the operation, it has the chance to repair perhaps laparoscopically and during recovery.
Otherwise, unknown oesophageal perforation may result a severe complication, even death.
In the investigation of the AFC [18], 13 oesophageal perforations have been reported, and 9 were diagnosed intraoperatively, requiring 6 times a conversion. The diagnosis of the other four cases is done within 1–25 days. In 12 cases, the suites were simples. One death has been reported in a patient of 48 years, operated for a complete fundoplication, and, in which the removal of the valve was made by thoracic approach. All oesophageal wounds were sutured, three laparoscopically. A wound of the oesophagus occurred during the passage of tube Faucher (Table 3.2).
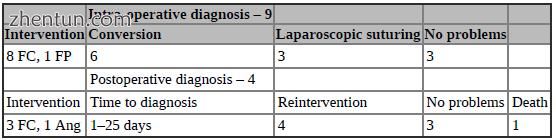
Table 3.2 Complications/wounds of the oesophagus, in the AFC study [18]
Prevention: Especially when there is the higher risk of oesophageal perforation, this can be minimised by the way retro-oesophageal dissection is performed, remaining in contact with the pillars of the diaphragm.
To avoid puncturing the oesophagus, we must not forget the basic principles of anti-reflux surgery: “Dissection of the oesophageal hiatus and not of the oesophagus”. Most importantly, do pay lots of attention to not let go unnoticed any possible injury, in order to not run the risk of a complication that can be catastrophic.
3.2.3.4 Gastric Perforation
Gastric perforations are rarer than oesophagus’s. Literature reports a certain number of cases. The series of Watson [20] reports 1 case out of 200, the series of Champault [15] reports 2 cases out of 940 and Hinder’s reports 5 cases out of 2453 [19].
In AFC’s [18] series, of the 12 gastric wounds reported 3 were pre-operatively discovered and treated; two with sutures and one by a secondary gastrectomy. Nine were postoperatively found, with two necrosis. Six suturing repair and three gastrectomies were performed. One death has been reported in connection with this complication (Table 3.3).
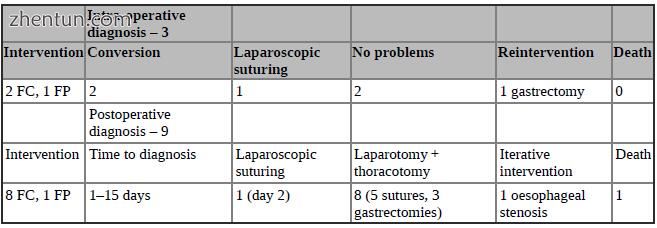
Table 3.3 Complications/gastric wounds, in the series of the AFC [18]
3.2.3.5 Complications: Gastric Wounds
Usually the location is anterior, near the greater curvature. Rarely, it is torn by excessive tension of the valve. In this case, the location can be posterior on the valve, retro-oesophageal, close to the pillars. It can also happen as a perforation of the gastric fundus during the difficult dissection in complicated interventions REDO (Video 3.4).
Video 3.4: Gastric perforation of the fundus, during dissection in a REDO surgery
Other rare event of perforation has been described, on the large gastric tuberosity, because of rough use of traumatic forceps. This type of perforation is easier to recognise and can, often, be repaired by laparoscopy [21]. It is also reported in literature, the ischaemic perforation of the great tuberosity due to extensive gastrolysis. Excessive section of short vessels can lead to shortness of blood supply to the great tuberosity relying on the posterior gastric artery whose anatomical variability does not provide for sufficient substitution vessels [22].
3.2.3.6 “Gaseous” Complications
Gaseous complications are represented by the pneumothorax and the pneumomediastinum.
The pneumomediastinum is a specific complication of any laparoscopic surgery with opening of the lower mediastinum (GERD, Heller, vagotomy, etc.). Most often it is also because, during this extensive dissection, there was an association with high abdominal pressure. But all patients with dissection pushed into the lower mediastinum and in whom there is high abdominal pressure do not have, systematically, a pneumomediastinum. This mechanism is not the only
cause to explain the pneumomediastinum. Perhaps there is an anatomical reason?
The pneumothorax is defined by the passage of CO2 into the pleural cavity through a pleural breach. It is not always the result of the operative act. Decreased oxygen saturation, increased airway pressure and, in particular, abnormal movement of the hemidiaphragm can be called signs of pneumothorax. The diagnosis is made by the analysis of the pleural gas where CO2 can be found.
Joris [23] noted that a capnothorax can be bilateral. Usually, it is well tolerated but it should be treated early. Finally, he showed that PEEP is the most efficient treatment, while it is contraindicated in pneumothorax.
These complications are, in fact, very frequent and less serious.
Pneumothorax requires:
A pleuropulmonary breach during surgery
A rupture of an emphysema bullous by increased pressure in the airways
Pleural wounds most often affect the left pleura. The main mechanism is the extensive dissection in the lower part of the mediastinum and going through the wrong retro-oesophageal plan during the dissection of the left side (Video 3.5).
Video 3.5: Pleural wound during mediastinal dissection
3.2.3.7 Other Complications
Some anecdotal complications are increasingly reported:
Cardiac dysrhythmia attributed to a direct myocardial injury [24]
Acute myopericarditis mechanism [25]
Cardiac tamponade by wound in the right ventricle [26]
Some specific technical complications have been published in the literature, as some cases of splenic infarction (3 %) (Video 3.6) or very rare cases of necrosis of the gastric valve (0–0.5 %) after section of the short vessels during a Nissen [27–29].
Video 3.6: Partial splenic infarction
3.3 Guide to Prevention and Management of Intra-operative Complications
Prevention of complications is the best treatment. Only perfect planning and excellent execution of the technique can minimise complications and their sequelae.
Surgical complications of laparoscopic techniques for GERD are, in general, due to non-compliance with well-standardised surgical steps.
The risk of complications and failure may decrease considerably if there is:
A correct indication
Good choice of techniques
The respect for surgical principles and well-standardised rules
For this reason, we describe, step by step, a classical laparoscopic Nissen operation, emphasising basic principles of anti-reflux surgery and identifying critical technical points.
3.3.1 Operating Phases of the Typical Anti-reflux Surgery
Step-1: Dissection of the gastro-oesophageal junction
Step-2: Dissection and mobilisation of the oesophagus
Step-3: Preparation and mobilisation of the gastric fundus
Step-4. Approximation of diaphragmatic pillars (cruroplasty)
Step-5: Creation of the fundus valve (fundoplication)
3.3.1.1 Step-1: Dissection of the Gastro-Oesophageal Junction
Best Exposure of Hiatal Area
First step of the intervention is to have a good exposure in the hiatal region; for this, a liver retractor is used to lift the left lobe of the liver in order to get a broad view and a perfect exposure.
Remark: For work in the hiatal region, to have a good liver retractor is indispensable. The choice of the retractor and its good handling is important. During surgery, a mechanical arm fixed to the right of the operating table, in order to get long-time stability, can hold it.
Risk: Liver haemorrhage Mechanism: Inappropriate retractor, careless use
Prevention: Select a special atraumatic retractor for the liver, place it carefully and monitor the position during surgery (Fig. 3.1).
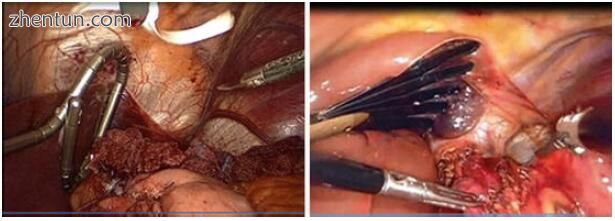
Fig. 3.1 Two different types of liver retractors
Best Position of the Working Area
After having installed the liver retractor and obtained a correct working area, the assistant seizes the stomach under the oeso-gastric junction with a grasper and pulls it down and to the left. The gastro-oesophageal junction should remain tense by the pull on that forceps for the security and efficiency of the dissection.
Remark: The caudal and leftwards traction of cardia with an atraumatic and appropriate grasper is essential to effective work.
Risk: Laceration or even perforation of the stomach.
Mechanism: Use a traumatic grasper and pull excessively and without care and attention.
Prevention: Use only an atraumatic grasper to hold on the cardia and draw up the necessary requirements.
Opening of the Lesser Omentum and Access to the Right Crus
After good exposure, the lesser omentum is to be sectioned, to allow access to the right crus of the diaphragm. The pars flaccida and pars condensa of the lesser omentum are incised by, at the same time, targeting the upper part of the right crus, which is an essential referral point, before addressing the dissection of the back part of the oesophagus. It is, often, under question whether to preserve or to cut the left hepatic artery which, often, accompanies a left hepatic vagus nerve (Fig. 3.2).
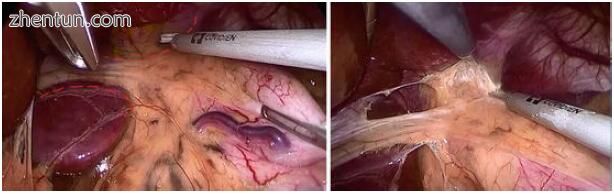
Fig. 3.2 The large size of the left hepatic artery vagus nerve are preserved
Remark; These branches of artery and nerve pass horizontally in the middle of the working field and divide it in two compartments. If it is not cut, working through the upper or lower window of this space will not be very easy.
Recommendation: It is recommended, if possible, to preserve a big size artery, without cutting it, even if it makes the approach to the area difficult. If it does not seem very important, this slim branch in the omentum may be cut between two points of haemostasis in order to have suitable working fields. Conversely, if there is an artery of big size, it is advisable not to cut it, even if it makes the approach to the hiatus harder. In the case of a very thin patient, this is not a problem, but, sometimes, in more obese patients, it is hard to find the crus; so, maybe it is quite helpful to look from below. Meanwhile, this window must be large enough just to admit the fundoplication wrap.
Risk: Section of a large artery without effective haemostasis may be a cause of important bleeding (Video 3.2).
Prevention: If the left hepatic artery is large, it must be, effectively controlled, with ligatures, clips or proper devices as LigaSure or Ultrasonic Dissector.
Access the Cardio-oesophageal Junction
The dissection of the cardio-oesophageal junction begins by opening the peritoneal layer of the phreno-oesophageal ligament at the base of the right crus and extends upwardly at its inner edge. This step allows to identify the essential structures: the crura, the vagus nerves, the abdominal part of oesophagus, the mediastinal pleura, the VCI and the aorta.
Remark: In some cases, it can show the existence of an annoyingly and significantly sized lipoma at the hiatus; this can make dissection difficult.
Dissection extending up to the inner edge of the crus must not damage the peritoneum covering it, in order to preserve its strength during subsequent rapprochement of the pillars.
Risk: The existence of a significantly sized lipoma can prevent the making of a proper fundoplication and can lead to annoying postoperative dysphagia.
Inattentive and deep dissection on the pillars can damage the muscle sheath. This will be a factor in the weakness of the cruroraphy and may lead to postoperative tearing with recurrence of the situation.
Prevention: If the size of the hiatal lipoma is important, it is advisable to resect it at the beginning of the dissection; this will allow easy dissection, the creation of a correct fundoplication and the avoidance of an eventual dysphagia after surgery (Fig. 3.3).

Fig. 3.3 Dissection of the large-sized lipoma at the hiatus
Dissection gestures on the pillars must be superficial in order for the sheath of the pillar muscles to remain intact.
Dissection of the Phreno-oesophageal Ligament
The upper part of the phreno-oesophageal membrane is to be opened transversely, from right to left until the left crus. The dissection can individualise the right edge of the oesophagus and the posterior vagus nerve.
Remark: In this step, a blunt dissection, the verification trunks of anterior and posterior vagus nerve is recommended.
Risk: Injury of the oesophageal layer, perforation or section of the vagus nerve.
Prevention: This liberation should be very careful and divide the superficial layer of the phreno-oesophageal ligament to avoid injury to some structures at the anterior aspect of the oesophagus, such as the vagus trunk.
3.3.1.2 Step-2: Dissection and Mobilisation of the Oesophagus
An incision of the phreno-oesophageal membrane is continued on the medial
relief of the right crus, from right to left. The section of the upper part of the gastrophrenic ligament, along the left crus, facilitates the next step (Fig. 3.4). Dissection progresses from inside to outside in front of the left crus until the upper pole of the spleen is identified (Fig. 3.5).
Figs. 3.4, 3.5, and 3.6 Dissection and mobilisation of the oesophagus
A tape is passed around the oesophago-gastric junction. The traction towards the bottom and outside will help to dissect the lower part of the oesophagus. The dissection around the oesophagus continues into the mediastinum (Fig. 3.6).
Recommendation: The left crus must be released as far as possible in order to create an appropriate retro-oesophageal passage; this needs to be wide enough to allow subsequent passage of the anti-reflux valve.
Lifting the gastro-oesophageal junction with a tape allows avoidance of any traumatic grasping of the organs and helps mobilisation of the gastro-oesophageal junction in different directions. It also serves as a landmark to assess the oesophageal segment length below the diaphragm.
Mobilisation of the lower oesophagus must be over a length of 5–10 cm for having an infra-diaphragmatic oesophageal segment length of 2–3 cm, without traction.
The vagus nerves must, systematically, be identified and protected. Remark: The dissection of the hiatus and lower part of the oesophagus into
the mediastinum could be often very delicate. The division of the posterior attachments of the cardia on the diaphragm allows to enlarge the retro-oesophageal window. A left diaphragmatic artery can be found crossing through that space, in some cases, and this must be kept in mind.
Risks: Perforation of the oesophagus, pneumothorax and bleeding if dissection is not careful.
Prevention: The rule of “dissection first of the oesophageal hiatus and not of the oesophagus” must be respected to avoid any oesophageal perforation. This risk can be minimised by retro-oesophageal dissection in contact with the crura. If there is a large diaphragmatic artery or other unusual vessels, they must be carefully dissected, coagulated or clipped to avoid an undesirable haemorrhage that makes difficult to continue the dissection at this closed and deep area.
Intra-mediastinal dissection shall be done under direct vision, not blindly, preferably with a 30 or 45° optic, and it shall be sufficiently large although not too excessive, in order to avoid negative effects. The pleura shall also be viewed and protected during dissection, to avoid a tear that can lead to a pneumothorax (Fig. 3.7).
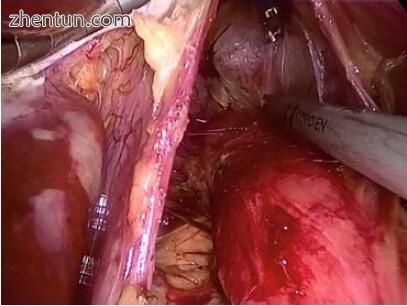
Fig. 3.7 The pleura shall be protected during the intra-mediastinal dissection
3.3.1.3 Step-3: Preparation and Mobilisation of the Gastric Fundus
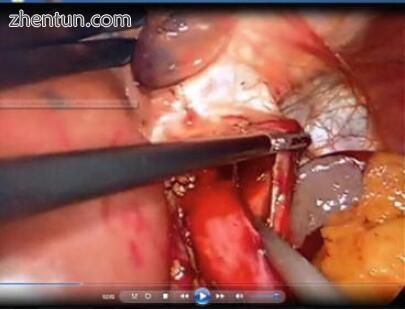
This step involves mobilisation of the gastric fundus, which is used to create the anti-reflux valve. This requires the section of the gastrosplenic ligament and the first short vessels (Fig. 3.8).
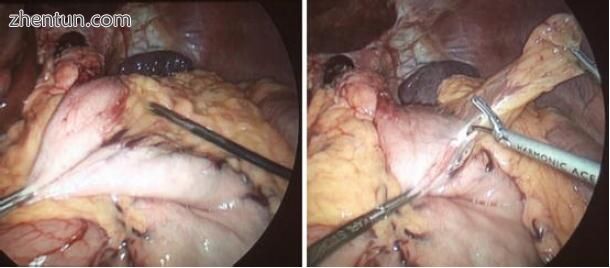
Fig. 3.8 Section of gastrosplenic ligament with the first short vessels
Remark: The systematic section of the short gastric vessels is to enable the realisation of a tension-free valve (floppy Nissen). Otherwise, if the technique used is the Nissen-Rossetti, it does not require this cutting.
Recommendation: This division shall only concern some of the short vessels, not all of the great curvature. Only three or four of the superior short gastric vessels need to be severed; an extensive release of the large curvature of the stomach starting to lower the pole of the spleen is not desirable. The dissection shall continue to the left crus, to liberate the posterior side of the fundus. In certain cases, division of the posterior fundic artery maybe necessary.
Monopolar or bipolar cautery, clips, ultrasonic scissors or a vessel sealing device may be used to cut and divide the short gastric vessels.
Landmarks-1 (Dr. Cadiére) [30]; Dissection of gastrosplenic ligament starts at where the short vessels stop orienting towards the transverse colon (EMC 1995).
Landmarks-2, (Dr. Dallemagne) [11]: The ligament is first divided in its cephalad origin where some fat folds may be found (WebSurg), (J Coeliochir).
Risks: Injury to the spleen, bleeding.
Prevention: Dissection of short gastric vessels must be very careful, especially in obese patients. A short gastric vessel poorly controlled may cause local bleeding diffusing into the gastrophrenic ligament and make the following mobilisation difficult. The use of modern haemostatic instruments considerably facilitates a secure haemostasis.
3.3.1.4 Step-4. Approximation of Diaphragmatic Pillars (Cruroplasty)
Systematic approximation of the pillars is essential. It not only contributes to restoring one of the elements of the anti-reflux barrier but also stabilises the anti-reflux valve inside the abdominal cavity and prevents the appearance of a para-oesophageal hernia (Fig. 3.9).
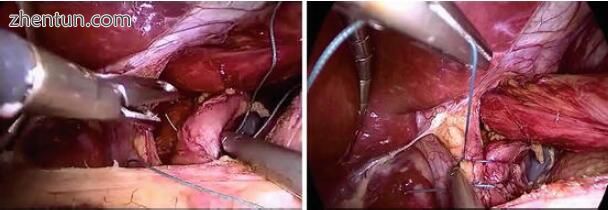
Fig. 3.9 Approximation of diaphragmatic pillars (cruroplasty)
Hiatal repair with mesh reinforcement may reduce hernia recurrence, especially in patients with a large hiatal hernia or in a complex REDO surgery. However, mesh-related complications have to be considered (Fig. 3.10), (Video 3.7).
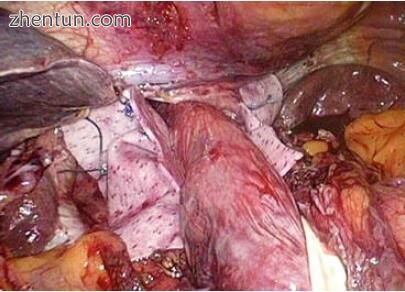
Fig. 3.10 Hiatal repair with mesh
Video 3.7: Hiatal repair with mesh
Remarks: Closure of the crus can be done in front or behind of the oesophagus. Posterior closure seems more anatomical. Anterior closure may be used in cases of very large hiatal defects, but it involves sutures under high
tension. In those cases, it is when there may be some interest in the use of mesh reinforcement as a possible solution. However, mesh-related complications have to be considered.
Indeed, significant and persistent postoperative dysphagia is often due to a too tight closure of the pillars. This may become a valve problem (EMC-3).
Two or three points of interrupted non-absorbable sutures of 0 or 2/0 are usually sufficient to assure proper repair the hiatal defect posterior to the oesophagus.
Recommendation: At the beginning of surgeon’s experience, it is recommended to place a 55 French “bougie” into the oesophagus to avoid strangulation, which will result in a dysphagia.
Risks:
Haemorrhage by lesion of the VCI or the aorta
Laceration of the crus by too tight sutures
Immediate dysphagia due to a too tight closure of the pillars
Prevention: Be careful, by placing the first point inferior; do not touch the aorta when dealing with the left crus or the inferior vena cava when dealing with the right crus (Fig. 3.11).
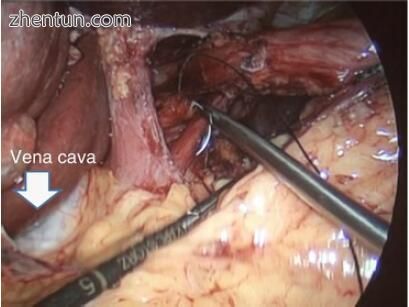
Fig. 3.11 Be careful not to hurt the inferior vena cava by loading the right crus
The sutures on the pillars should not be too tight to avoid laceration on the muscle fibres; these can lead to recurrence. Just approaching the crus shall be sufficient and effective.
An instrument of 10 cm—the width of a finger—introduced without difficulty between the oesophagus and the last suture ensures that the closure of the crus is not stenotic.
At the beginning of surgeon’s experience, it is recommended to place a 55 French “bougie” into the oesophagus to accurately size the oesophagus and to avoid any strangulation, which will result in dysphagia. But utmost care is necessary to avoid oesophageal perforation!!!
The placement of an oesophageal dilator during the creation of laparoscopic fundoplication is advisable as it leads to decreased postoperative dysphagia but should be weighed against a small risk of oesophageal injury. A 56 French “bougie” has been found effective but the evidence is limited.
3.3.1.5 Step-5: Creation of the Fundus Valve (Fundoplication)
The last step of the operation is the creation and fixation of the anti-reflux valve. The posterior-superior part of the gastric fundus is brought to the right of the
oesophagus through the posterior oesophageal window. The two parts of the valve are to be united in the anterior surface of the oesophagus by three non-absorbable sutures (Fig. 3.12).
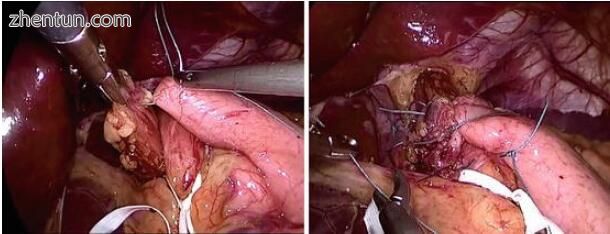
Fig. 3.12 Creation of the fundus valve (fundoplication)
Remarks
If a proper dissection was done to get a large retro-oesophageal window and adequate mobilisation of the large curvature, this valve will move easily through this retro-oesophageal window and will be maintained without any traction.
Recommendation
Verification of the absence of tension and play in the valve by the “bath towel movement” (go-and-back) in the posterior area.
The valve should be positioned at the level of the Z line, 1–1.5 cm above the anatomical junction.
The best length of the valve is about 2 cm in the case of a floppy Nissen.
It is important to have a good anchorage of the fundoplication on the gastro-oesophageal junction; otherwise it can slip rapidly.
The placement of an oesophageal dilator during the creation of a laparoscopic fundoplication is advisable as it leads to decreased postoperative dysphagia.
The valve must be fixed to avoid slipping, usually by two sutures which pass the anterior wall of the oesophagus and at the right of the anterior vagus nerve.
Risks: The placement of a 50–60 French “bougie” can be effective but must be balanced with a low risk of oesophageal injury due to lack of care when placing it into the oesophagus.
Prevention
One or two sutures passing the anterior wall of the oesophagus to prevent an eventual slipping into the thorax must fix the valve.
During this fixation, be careful to avoid taking within the suture the branches of the anterior vagus nerve; this may cause vagal damage.
The valve can be fixed also to the phreno-oesophageal ligament in order to give good anchorage to the fundoplication.
When the anaesthetist pushes the dilator in the oesophagus, do not forget to release the tape retractors at the cardia, to avoid a possible perforation of the oesophagus.
3.4 Postoperative Complications: Failures
According to Guidelines of SAGES (Society of American Gastrointestinal and Endoscopic Surgeons) [31], there is a failure rate of 10–15 % in spite of a successful outcome in 85–90 % of patients up to 5 years after primary anti-reflux surgery. Failure is usually defined as persistent, recurrent or new-onset symptoms.
The main symptoms of failure are:
Recurrent reflux symptoms
Gas-bloat syndrome
Dysphagia
3.4.1 Recurrent Reflux Symptoms
Persistent and recurrent reflux can be due to intrathoracic wrap migration, disruption of the wrap, slipping and/or telescoping. Recurrent reflux symptoms such as heartburn and regurgitation are the main complaints after unsuccessful anti-reflux surgery and are found in 61 % of patients with failure [32].
A variety of symptoms as inability to belch, gastric fullness, early satiety, diarrhoea, nausea and vomiting can occur postoperatively; some due to an overly tight wrap or an overly tight crural repair, others secondary to vagal damage.
3.4.2 Gas-Bloat Syndrome
The gas-bloat syndrome corresponds to a series of symptoms attributed to the inability to belch. The main complaint is postprandial bloating. Several factors are evoked to explain this symptomatology as the inability of the oeso-gastric junction to open in response to gastric distension. Some are caused by an overly tight wrap or by an overly tight crural repair. Iatrogenic vagus nerve damage causing gastroparesis can also cause this kind of symptoms.
3.4.3 Dysphagia
Troublesome dysphagia is the other most frequent symptom in failed anti-reflux surgery.
Dysphagia for solid food is common in the early postoperative period. This is probably dysphagia caused by the operative oedema, and it disappears spontaneously, often, in two or three months. This is functional rather than mechanical and, as such, does not need surgical correction. It is influenced by the ability of the patient to control his/hers emotions and eating habits.
One of the reasons for functional failure after primary anti-reflux surgery is misdiagnosis. These patients frequently have a primary functional disorder other than GERD such as achalasia, diffuse oesophageal spasm, nutcracker oesophagus, eosinophilic oesophagitis or scleroderma. Another possible cause for failure after primary anti-reflux surgery is that a wrong procedure was used in patients with severe oesophageal dysmotility or motility disorder.
If the intensity of dysphagia does not decrease after the third month and does not disappear, at the sixth month, it must be considered as a mechanical dysphagia, and this requires surgical correction. Accurate diagnosis must be made before any surgery.
Severe dysphagia requires early endoscopic exploration and, whenever appropriate, endoscopic dilation. If symptoms persist, revision surgery has to be envisaged.
The causes of persistent dysphagia can be intrathoracic wrap migration, slipping, telescoping, para-oesophageal herniation, mesh migration, excessive fibrosis (mesh-related or not) and/or an overly tight wrap or overly tight crural repair.
Excessive dysphagia and intractable pain and/or dyspnoea in the early postoperative course require immediate revision after appropriate investigations. In all other failure scenarios, the first-line therapy should be medical and/or supportive.
3.4.4 Some Remarks
3.4.4.1 Postoperative “Diaphragmatic Stressors”
One study has suggested that early postoperative gagging, belching and vomiting (especially when associated with gagging) are predisposing factors for anatomical failure and the need for revision [33].
In addition, hiatal hernias >3 cm at original operation have been reported to be predictors for anatomic failure.
3.4.4.2 Psychological Disease and Intervention
One study concluded that a 270° partial fundoplication had better outcomes in patients with major depression compared with a 360° fundoplication due to a lower incidence of postoperative dysphagia and gas-bloat syndrome [34].
3.4.4.3 Oesophageal Function
Patients with nonspecific spastic oesophageal motor disorders (such as nutcracker oesophagus, hypertensive LES syndrome) have been reported to be at increased risk for postoperative heartburn, regurgitation and dysphagia after a 360° wrap [35].
Symptoms should be the primary indication for any redo anti-reflux surgery. All patients seeking treatment for symptomatic failure after anti-reflux surgery
should be evaluated to identify possible causes of failure. Investigative techniques include endoscopy, manometry, oesophageal 24-h pH monitoring, barium studies and scintigraphy.
3.5 REDO
Redo anti-reflux surgery is required in 3–6 % of all patients who undergo primary anti-reflux surgery and should always begin with a clear definition of the anatomy [1].
Anatomical alterations such as recurrent hernia or a bilobed and twisted stomach have been described as reasons for failure and subsequent redo anti-reflux surgery. However, anatomical disturbance without symptoms should never be the only reason for redo surgery. Symptoms should be the primary indication for redo anti-reflux surgery. Conversely, postoperative anatomy as evaluated by endoscopy and/or barium studies can be normal in patients who still have symptoms.
Anatomical changes after laparoscopic anti-reflux procedures can be classified into several categories, including intrathoracic wrap migration, wrap disruption, telescoping, para-oesophageal herniation, a tight wrap or a tight crural repair and a bilobed or twisted stomach. In the case of any of these conditions, there has to be careful anatomical dissection and proper rearrangement before creating a new fundoplication.
Revisional surgery should be performed by specialised gastrointestinal surgeons with extensive experience in the field, in a high-volume centre. The surgeon’s technical armamentarium for revisional surgery should include all laparoscopic, endoscopic and thoracoscopic procedures (Collis), as well as all open procedures, including major resections, if they seem necessary to solve the problem.
3.6 Summary
Today, the laparoscopic anti-reflux surgery is the treatment of choice for GERD, and all types of fundoplication can be carried out in good conditions, in accordance with well-defined rules.
Surgical complications of the laparoscopic techniques for GERD are generally rare and due to the non-compliance with well-standardised rules, also lack of experience of the operator. In the beginning, during the initial learning phase, this is one of the main risk factors for complications [13].
Complications of laparoscopic treatment of GERD can be classified as preoperative (minor or serious) and postoperative failures (immediate or delayed).
Intra-operative complications of laparoscopic anti-reflux procedures are essentially traumatic and involve mainly the oesophagus, stomach, pleura and vessels, with consequent haemorrhage, perforations, pneumothorax and some other less frequent.
Haemorrhagic complications are rarely reported in the literature and usually without vital impact (rare cause of conversions and transfusions), whereas perforation of hollow organs as stomach and especially oesophagus can be more important, even catastrophic.
The risk of oesophageal perforation can be minimised by the retro-oesophageal dissection remaining in contact with the pillars of the diaphragm. To avoid perforation, we must not forget the basic principles of “Dissection at start of the oesophageal hiatus and not of oesophagus”.
The consequences vary as detection is early or late. If it is discovered during surgery, there is a good chance to repair, perhaps laparoscopically, with good recovery. Otherwise, with unnoticed oesophageal perforation, all of it can lead to a very severe complication, even death.
Gastric perforations are rarer than oesophageal, while pneumothorax and the pneumomediastinum are in fact very frequent and less serious complications.
Postoperative complications depend on a good diagnostic, choice of an adequate technique, experience and skills of the surgeon and the general condition of each case. The main symptoms of failure are recurrent reflux, gas-bloat syndrome and dysphagia.
Heartburn and regurgitation are the main complaints after unsuccessful anti-reflux surgery and are found in the majority of patients with unsuccessful result. Persistent and recurrent reflux can be due to intrathoracic wrap migration, disruption of the wrap, slipping and/or telescoping.
The gas-bloat syndrome corresponds to a series of symptoms attributed to the inability to belch. Some can be due to an overly tight wrap or an overly tight crural repair, others secondary to iatrogenic vagal damage.
Troublesome dysphagia is the other most frequent symptom in failed anti-reflux surgery. Dysphagia for solid food is common in early postoperative period. This is probably the dysphagia consequence of operative oedema as it disappears often spontaneously in 2 or 3 months. If the degree of dysphagia does not decrease after the third month and does not disappear by the sixth month, it must be considered as a mechanical dysphagia that requires surgical correction. This may be after some trial of endoscopic dilation.
参考:Complications in Laparoscopic Surgery A Guide to Prevention and Management |