2.1 Problem
Lesions of the biliary tract can happen during the performance of different types of surgery, not only biliary surgery itself. Mainly – although other much rarer options can happen – five types of surgery are responsible for these events:
Biliary surgery
Liver surgery
Portal hypertension surgery
Pancreatic surgery
Gastric surgery
In these types of surgery, sometimes dissection can be difficult, and the surgeon may lose the anatomic landmarks, becoming closer to causing lesions by dissecting and cutting tissue in the areas where the main anatomical structures are, because of not being aware of their real position.
Processes with a serious inflammatory reaction, or the ones which involve large tumours or collateral circulation, or, also very frequently, reoperations causing adhesions and distortion of the local anatomy, make the whole surgical
work in that field much more prone to lesions.
Going into a more detailed approach, let us start by looking at the most common biliary surgery performed: cholecystectomy. Our text will be directed at this type of surgery. Some studies rate this problem of iatrogenic lesions at a high stake, but these figures depend on the detail the surgical community relies on in finding complications and how these are graded; a multicentre study, for instance, of 24.800 patients, relates “post-cholecystectomy symptoms” from 12 to 68 %, and, depending on the centres reporting, serious complications were from 3 to 32 %. These figures show immediately that local approach and reporting are extremely variable and can cause confusion.
Nevertheless, reported rates of morbidity and mortality from cholecystectomy are not very different with the passage of years. Several series show this, with morbidity between 3.8 and 4.9 % and mortality from 0 to 1.8 % [1–3]. In these series, it is noted that a remarkable difference exists in the morbidity and mortality results, dependent, for example, on the age of patients; patients below 65 years of age have much lower mortality rates, for instance [3].
Bile duct injuries (BDI) keep having high incidence, despite all interest given and “calls for attention” which are being made so frequently. Very recently, SAGES set up a “task force” with the task of educating USA surgeons trying to obtain lower rates of lesions (“Safe Cholecystectomy Program”). These rates vary between less than 0.2 and 0.8 % and even more in “normal” cholecystectomies. But, if surgery was performed because of acute cholecystitis, these values are higher.
Even more so, in the difficult cases, leading to “conversion to open”. These, interestingly, show very high rates of lesions despite this conversion, which would, in theory, give better “view” to the operating field.
Within cholecystectomy, still the types of complications vary between biliary and non-biliary. Another multicentre study, covering 34.500 patients, showed the following complications and rates, post-cholecystectomy (Table 2.1):
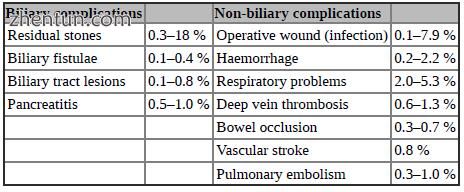
Table 2.1
On the whole, a little less than the previous mentioned ones, it is necessary to consider that some patients have more than one complication.
Non-biliary complications are the usual ones, known in general, and possible in any case of abdominal surgery; we are not going to talk about it in this chapter, concentrating our comments on the biliary ones and, amongst these, in the iatrogenic lesions to the biliary tract. These can be detected immediately, during surgery, in the early postoperative period or late, sometimes even months after surgery. What is also important is that about 2/3 of these lesions are not detected during surgery.
Nevertheless, we have to mention that some haemorrhage can be avoided by paying special attention to local factors: for instance, patients with coagulation disturbances or with portal hypertension may have to be dealt with by different solutions like a partial Torek’s cholecystectomy. In addition, the draining vein running within liver parenchyma, sometimes rather superficial, in the gallbladder bed, shall be avoided by taking all necessary steps not to go deep during the lifting of the gallbladder from its liver bed [4] (Fig. 2.1). If bleeding comes from this vein, control may be hazardous. The gallbladder shall be dissected from its bed by “lifting” it and by simple separation, without being necessary to do any sharp cutting in general. In cases of acute cholecystitis or of strong adhesions after several inflammatory episodes, this may be necessary, but it is then when all surgeons shall be over attentive and when all cautious movements shall be put into practice.
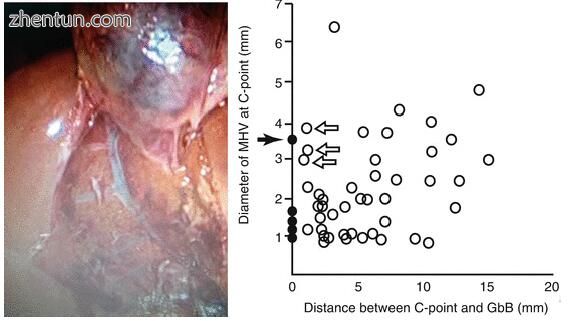
Fig. 2.1 Vein at gallbladder’s bed and its frequency of depth [4] (Photo – courtesy of Dr. Jaime Roque)
Obviously, it is supposed that elective patients have a complete workout, where alterations like abnormal blood clotting will be detected and proper measures taken.
Within the biliary complications, the contents of this chapter will focus mainly in the iatrogenic lesions.
2.2 Causes (“Why” It May Happen)
If we look at the possible causes of complications, we have several variables to consider. These depend on the patient’s general condition and comorbidities, on the type and seriousness of the disease, on the training and expertise of the surgeon, on the quality and existence of all pieces of equipment necessary and on the hospital environment.
Another frequently mentioned variable, in what concerns laparoscopic surgery, is the so-called learning curve. But, although this “learning curve” can be responsible for many things and has to be eliminated or minimised as much as possible, it has no defined causal relation to BDI; the “learning curve” for laparoscopic cholecystectomy goes well beyond 50 cases, and, although operating time keeps lowering until 200 cases, improvement in the cognitive skills to deal with difficult cases continues [5].
It has also been shown that the risk goes beyond “first cases”, as demonstrated in the following series from the same institution: first 1284 cases (0.58 % BDI) and next 1143 cases (0.50 % BDI) [6]. An enquiry into 1500 surgeons reports that about 30 % of BDI occur after the first 200 cases [7]. We can only conclude that surgeon’s experience does not minimise the risk.
This persistence of high rates of BDI after the initial training curve shows that there is a difference in these; it is considered that there is a difference between “experienced” surgeons and “experts”. “Experts” are surgeons with “consistently better outcomes” (namely, BDI rates, consistent and very low or close to zero).
Some local factors have shown to be responsible for a higher incidence of complications: local inflammation is a well-known one, even conditioning the timing of surgery for acute cholecystitis; fibrosis, reoperations with “changed” anatomy or urgent surgery are other causes. Also, local adhesions or bowel distension can be a reason.
Choice of wrong timing to operate acute cholecystitis is a common cause for surgical difficulties and eventually surgical accidents. There is evidence that performing cholecystectomy more than 5 or 6 days after the onset of the acute inflammation will make surgery much more difficult and face a great number of
serious inflammatory adhesions, causing much more bleeding than usual and making it difficult to recognise proper anatomy and surgical landmarks.
Some signs, visible previously to surgery or during it, shall lead to the suspicion that serious inflammation may be present; thick gallbladder wall (>5 mm) at US, firm adherence of gallbladder to omentum, duodenum, colon or stomach, liver pulled down around a shrunken gallbladder or when the surgeon cannot find the gallbladder are some of these.
Before following on to other possible causes, let us summarise patient’s ones. One must not forget who the high-risk patients for iatrogenic lesions are:
Male patients
Patients with cirrhosis or liver steatosis
Obese patients
Those having had previous upper abdominal surgeries
Those having delayed treatment of acute cholecystitis
A multitude of technical mishaps are causes for complications, most of them being present due to the ineptitudes of the surgical team and from some of its technical options: Bad ports positioning, in the case of laparoscopic approach, is an evident cause, but many times these are not properly weighed. By itself, or because of the above, a bad field exposition and bad illumination are also reasons for a higher incidence of complications. Too much smoke or too much blood in the field can hamper visibility to a point of danger.
There is a need to have the ports correctly positioned regarding the possible location of the gallbladder, patient’s BMI and configuration and size of the instruments being used.
In the same line, bad anaesthesia is a well-known factor by contributing to bad visualisation of the operating field; patient’s lack of relaxation will “close” the operating field.
Surgeon’s (or team’s) inexperience as well as surgeon’s (or team’s) tiredness are very often disregarded or not recognised. In connection with these factors is not knowing of eventual anomalies; these anomalies are frequent, well known and defined and represent a serious situation, which, if not recognised, give no excuses to the surgeons involved. No surgeon shall undertake any kind of surgery without minimal theoretical and practical preparation, much more so in the biliary field, where important anomalies are so frequent. On the other hand, also related to “experience”, surgeon’s overconfidence can be a cause of BDI, by “simplifying” some cases or some technical steps of surgery.
The surgeon can, still, be a cause of BDI, by not paying attention to some crucial points: performing surgery with a bad vision angle, using wrong instruments and applying wrong use of technologies are, too often, causes of lesions.
In a similar level, technical failures come as causes for complications; some of these are surgical technique failures, some instrumental ones. Inappropriate traction of structures, supposedly for “better exposition”, can alter the anatomical relations and be a cause of lesions; the same goes for undue use of diathermia, which, unfortunately, we see too often, either by using it too strongly or for too long. Another point for which care is mandatory relates to proper maintenance of instruments; especially reusable ones can have deficient isolation, giving rise to coupling lesions, when, while using electrosurgery, non-visible sparks jump from the instrument to organs away from vision, with consequent thermal lesions.
Instrumental mishaps are, sometimes, unavoidable, but their occurrence must be anticipated, and backup material and/or appropriate maintenance and repair are a must. Instruments can be broken, tipped or sharp pointed, can be inappropriate for the task or can mechanically malfunction.
Let us look at an important point related to these issues: human error. The so called “learning curve”, with its associated human error, which is so often used nowadays in surgery as an “explanation” for some complications, would never be accepted in high-technology industries or in some sensitive areas like airlines or military. Many mandatory preparation steps have been designed by these groups to impose rules and protocols, in order to minimise the problems; soon we may have to do the same and follow, for instance, a complete checklist procedure before and during each surgical operation; checklists are a controversial point to be discussed under a different approach. Training, on the other hand, is a capital issue and it is necessary to keep full attention to this sector.
Human errors can happen, nevertheless, despite all efforts to avoid them; we have to minimise them to the extreme. More often, they are based on technical, training or knowledge failures (ignorance) and with non-compliance to established rules. These are the ones “easier” to control. Others are related to a complex and not well-known phenomenon: visual failure or misguidance.
Included amongst processes called “heuristic”, human brain can induce visual errors that, no matter what further obvious changes there are in the visual field, become stable and understood as reality, staying like that for the whole surgery. This means that, under certain circumstances, anatomic structures are perceived as different ones in the beginning of the surgery (the most common one being interpreting the CBD as being the cystic duct), and the brain “keeps telling” that this first perception is the correct one, leading to the crucial iatrogenic lesion [8].
In a more practical example, this process can also be called “optical illusion” and is well exemplified in the two drawings below: in one, called the Kanizsa’s triangle, half of the viewers will see a black-lined triangle, the other half a white one; the other drawing will show six or seven cubes piled in different directions, again depending on the first view of the observer. As a matter of fact, in Kanizsa’s triangle, there is no triangle: just three angles and three “Packman drawings”, which, in togetherness, compose the image(s) that the brain “thinks” to be the right one (see Figs. 2.2 and 2.3).
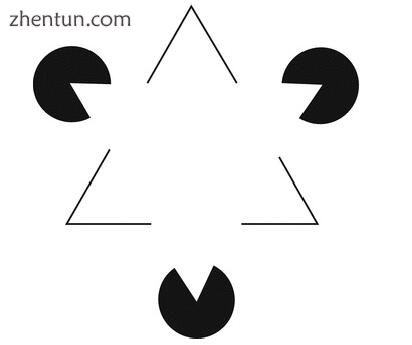
Fig. 2.2 Kanizsa’s triangle
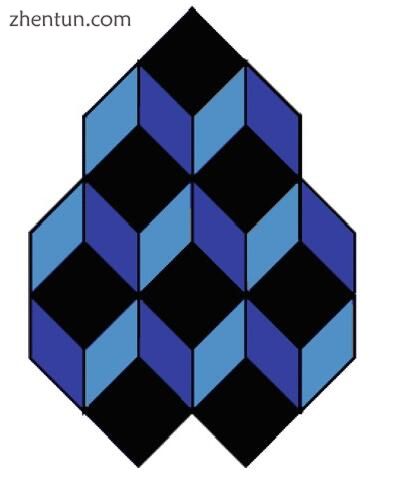
Fig. 2.3
Way and Lawrence have shown in 2003 that the great majority of iatrogenic lesions of the biliary tract (97 %) are caused by errors in visual perception and only 3 % because of technical errors (Fig. 2.4).
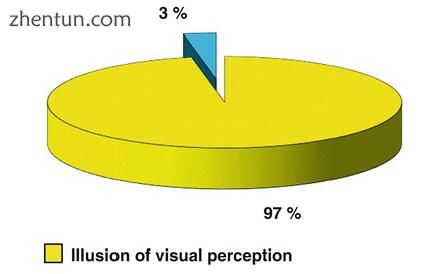
Fig. 2.4 Rate of technical (3 %) and non-technical (97 %) causes of errors leading to iatrogenic bile lesions
This means that most lesions are caused by “intentional” actions by surgeons (not realising it, evidently), leading to unintentional results. These errors of visual perception can be caused – besides the basic problem – by visual difficulties under special situations: inflammation, too much cephalic retraction and, at the same time, insufficient lateral retraction, and “camel hump” position of the CBD because of too much upper traction of the gallbladder infundibulum [9].
2.3 Prevention (with Tips and Tricks)
Many of the explanations for the “causes” are, at the same time, self-explaining regarding what has to be done for “prevention” of the complications.
We can consider that one of the most important issues, which allow minimisation of complications, is correct indication and preparation of patients for any given surgery. Fast-track is also a possibility for these patients, but let us not forget that the whole concept of fast-track does not allow “forgetting” to apply all necessary steps.
All these factors lead to “paradigms of avoidable error”, which are a challenge for every surgeon involved in biliary surgery.
The questions and paradigms are:
Can the use of a meticulous technique and of an intense effort to identify the anatomy avoid lesions?
It is known that prosecuting “excellency” can diminish the rate of complications, but can it ever avoid it completely?
Will the results of any working group or surgeon always be conditioned by statistical compilations?
Statistically, it can still be said that, despite all efforts, a lesion of the biliary tract will always occur, at least once during the career of any GI surgeon. Because of this, in the end, and the most important: are complications inevitable??
While the goal should really be minimising harm, this does not seem at the moment completely avoidable. Only a culture of prosecution of quality and excellence, using all means at our disposition and implementing checklists, protocols, compliance of rules and proper training, can lead, eventually, to ground zero of complications. Checklists, as mentioned before, are a subject to be discussed in detail elsewhere.
Strasberg has defended, for quite some time now, that the systematic use of the so-called “Critical View of Safety” (CVS) – his dissection technique – can prevent the occurrence of iatrogenic lesions; in some countries, it is mandatory to use this dissection approach and to provide evidence of its use, the best evidence being provided by images, either video or still photos [10]. CVS dissection consists of performing a dissection, which ends up by showing only two structures coming to the gallbladder fundus (cystic duct and cystic artery) (Fig. 2.5). This dissection technique has been favourably compared to the “funnel” one, also called “infundibular”, coming from above, which risks confusion between CBD and cystic duct. Nevertheless, CSV dissection can be pretty difficult to achieve in “the difficult” gallbladder. We believe that these cases demand a much more meticulous dissection, step-by-step until a close to CVS view can be obtained.
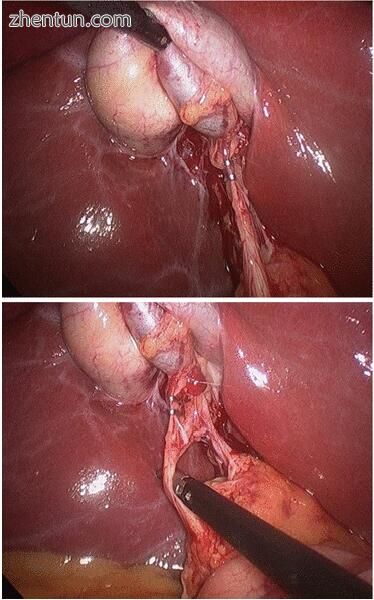
Fig. 2.5 On the left can be seen the positioning of clips in a tubular structure, after finishing dissection and before cutting the cystic duct. The photo on the right side shows the “Critical View of Safety”, in a case where the view could be misleading, with the cystic duct highly implanted. In this case, there was a risk of cutting, inadvertently, the common bile duct
2.3.1 Lesions of the Biliary Tract
These are the most serious, in general, complications in biliary surgery (as well as in other surgeries, as mentioned in the beginning). Many lines have been written about these lesions, when laparoscopic surgery became widespread, many of them calling attention to the problem and many implying that laparoscopic surgery was the culprit of all of it.
What seems to be true is that these lesions are more severe than the ones existing previously, in the times of “open” cholecystectomy [11].
Calling the attention to the problem, already in 1944, Grey Turner wrote in the “Lancet”: “CBD lesions are, almost always, a result of an accident during surgery, and, therefore, it can only be attributed to the surgical profession… … These lesions cannot be seen as a normal operative risk…”
The total rate is not high in global terms, but the real importance relates to the seriousness of these complications, mainly considering that its majority happens during surgery for benign situations (Table 2.2).
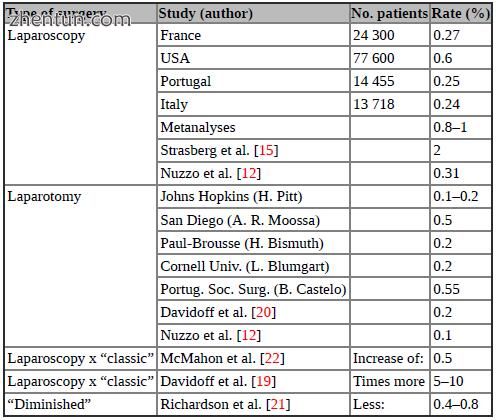
Table 2.2 Incidence of iatrogenic lesions of biliary tract
Some patients have specific causes for a higher possibility of lesions, either by their own comorbidities or by problems, errors or mistakes during surgery. Compromised healing in patients with bad nutrition status, cachexia or under treatment with steroids or immunosuppressors is one of the possible causes, and it shall be anticipated by the surgeon, before operation, bringing a serious state of alertness. Bactibilia, which may happen in up to 90 % of patients with acute cholecystitis, is another serious risk factor. Others may be cholangitis, gallbladder empyema, jaundice, CBD stones, acute cholecystitis and age above biliary tract lesions during surgery:
1. Dangerous disease – relating to situations where local surgical conditions convert the “surgical territory” into an area of difficult management because of inflammation, sclerosis, fibrosis or exuberant vascular territory, as it happens in cases of late acute cholecystitis or portal hypertension.
2. Dangerous anatomy – in the cases (about 10–15 %) where there are anatomic anomalies; it is necessary that the surgeon is well aware of the incidence and of the types of anomalies. While some are of no surgical importance, others can lead to catastrophe.
3. Dangerous surgery – although technical deficiencies can happen without warning, some others can be anticipated, and preventive measures can be applied. Surgery performed by surgeons or teams without proper physical or training conditions is another scenario leading to disaster.
Direct causes for biliary stenosis – early and late – are:
1. Tying, cutting or resecting the CBD
2. Luminal occlusion (total or partial, when tying the cystic duct – the “camel hump” situation)
3. Ischemia of CBD (too much dissection can cause this)
4. Periductal ischemia (same cause)
5. Luminal trauma while exploring
6. (Pre-existing benign stenosis – very rare nowadays)
All of these can happen without the awareness of the surgeon, mainly because of the reasons exposed above. Nevertheless, some measures can be applied before and during surgery, to prevent these lesions:
Surgical access shall be adapted to morphology – this can happen when a nonroutine placement of trocars is used; placement has to be chosen individually, according to the patient’s anatomy.
Good exposure of the hepato/duodenal space – by judicious use of patient’s positioning and traction of gallbladder’s fundus and neck. A movement with the forceps, forcing a “flag in the flagpole” display of cystic duct’s face, right, left and back views, will help in preventing lesions. The same applies to the Critical View of Safety dissection (Fig. 2.6).
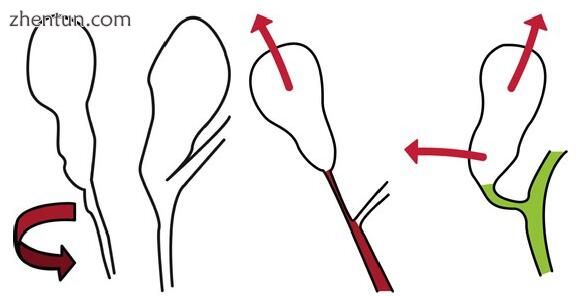
Fig. 2.6 These drawings show the importance of the execution of the “flagging” manoeuvre and of the proper directions of traction of the fundus and of the infundibulum of the gallbladder. “Flagging” and turning around the infundibulum can show the correct position of the CBD, avoiding the “hiding CBD syndrome”, which can be a major cause of a serious lesion (see Video 2.1). On the right side, it is shown how correct traction can help: retracting the infundibulum of the gallbladder to the right misaligns the cystic duct from the common bile duct showing clearly which is which
Also, too much traction in the gallbladder neck, and in the wrong direction, can pull the common bile duct from its normal location, causing the so-called “camel hump” position of the CBD at cystic channel insertion, leading to its inadvertent clipping and/or partial removal (Fig. 2.7).
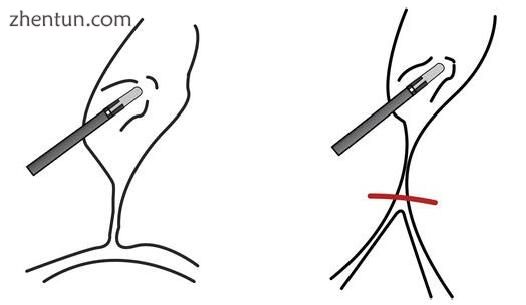
Fig. 2.7 Traction in the gallbladder, leading to “camel hump” position of the common bile duct; this can cause possible inadvertent clipping of the duct and/or partial removal (see Videos 2.2 and 2.3)
Good identification of structures, before tying, clipping and cutting – this is one of the most important steps in prevention, as we have mentioned, that only a certain constant rate of anatomical anomalies exist, but, in addition, the brain can “trick” the vision of the surgical field, inducing perception errors. Using mental checklists for identification of anatomy, with routines in following and showing some portions, and confirming them with the first aide are good measures to diminish this danger.
Appropriate dissection – follows the same cautions as above and implies the caution of not performing important and irreversible steps in surgery, without being absolutely sure of what is visible; do not “assume” anatomy and structures, and remember that inflammation and fibrosis can hide the correct planes of dissection.
If necessary, perform direct cholecystectomy – as a safety measure, and this applies for both types of surgery.
Selective cholangiography – it can be necessary to perform a cholangiography in certain cases, to clarify ductal anatomy; it is necessary to realise that cholangiography implies clipping and cutting the biliary tract and that this action in itself can be the cause of a lesion. The safest way to execute this exam, if one wants to see the anatomy of the biliary tract, is to do it through the gallbladder, before clipping the cystic duct. CBD’s puncture for performing the cholangiography can be the cause of postoperative bilomas. Some recent studies show that fluorescence cholangiography can be a very good and non-invasive alternative. As basic understanding, IOC (intraoperative cholangiography) does not avoid, by itself, biliary tract lesions [13].
Clamping of the pedicle, if big haemorrhage – another important tip; it is imperative, facing difficult bleeding or bleeding which is impossible to control immediately, to have a proper view of the origin of the haemorrhage and to evaluate its amount and possible ways to control it. This can only be done by stopping the blood flow, and this can be done by means of a clamp in the pedicle. There are ways to do this in laparoscopic surgery, but if the surgeon finds it difficult or too challenging, it is time to either ask for immediate help from someone with higher expertise or to convert. Shooting clips in a blind way to the area where the bleeding seems to come from leads very frequently to serious complications, even if the haemorrhage is controlled.
The fall of a clip from the cystic artery stump or its inadvertent cutting can, often, lead to a retraction of this stump, with profuse bleeding, behind the hepatic duct. Trying blindly to control this haemorrhage by clips can cause hepatic duct lesions in the area shown in Fig. 2.8.

Fig. 2.8 Artery’s retraction behind hepatic duct can be a cause of lesion if the attempts to control it are done blindly
Great care with the use of electrosurgery – despite all attention, electrical current follows structures and directions, which the surgeon is often unaware of. Conduction of electricity burns through ductal structures can cause extremely serious and very extensive lesions, sometimes destroying almost the whole extent of the main bile duct. Also, minute problems in the protection layer of certain instruments can give rise to sparks, injuring areas out of sight (the “coupling” problem already mentioned) (see Videos 2.3 and 2.4).
This brings to discussion a question many put: Are the lesions from laparoscopic surgery more serious?
The fact is, in laparoscopic surgery, some lesions started to show, which did not happen before; these are the lesions caused by total destruction of the CBD, for instance, because of extensive or wrong use of electrosurgery and the ones which imply removal, erroneously, of long lengths of the biliary tract. There has been the implication, by some authors, that some more recent surgical series,
regarding treatment of CBI, have a slightly inferior success rate than older ones; this might be due to the existence of worse lesions in the laparoscopic era. As a matter of fact, about 30 % of lesions, nowadays, are extensive burn lesions.
Another type of lesion relates to resection (or excision) of extensive length of the biliary tract. Lesions often very close to the hilum happen a lot as well as their coexistence with biliary fistulae, with consequent increase of inflammation, because of bile action. All these in togetherness with the fact that in many other cases we see bile ducts with small calibre are reasons for the increase of the seriousness of the injuries (Fig. 2.9).
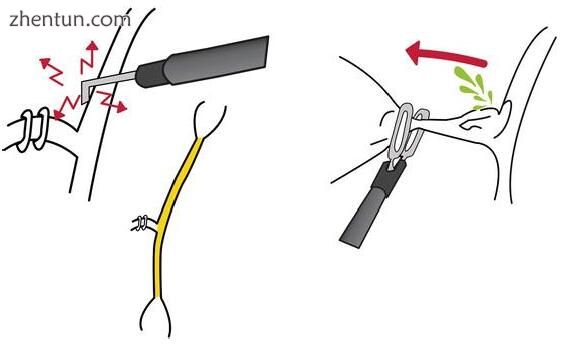
Fig. 2.9 Thermal lesions cause extensive damage of the bile tract, and rough manipulation can be the reason for large defects of bile ducts (see Video 2.5)
Alternatively, some other lesions are also more benign, like tangential lesions, clip falling or puncture lesions, allowing treatment by minimally aggressive endoscopic methods. Injuries can be graded, from less to more severe, as:
1. Puncture
2. Partial laceration
3. Complete section
4. Obstructing clip
5. Enlarged section (tissue removal)
6. Thermal lesion
7. Thermal necrosis
Some of the less severe can be approached and treated only by endoscopic methods.
More recommendations can be given regarding attitudes to minimise BDI. It is necessary for surgeons to keep some technical details in mind, and the permanent use of “prevention” measures, even in the “simplest” surgery setting. Always do a surgical access, adapted to the patient’s morphology, giving a good
exposure of the hepato/duodenal space and having good identification of structures, before tying or cutting anything. Appropriate dissection and, if necessary, direct cholecystectomy and/or selective cholangiography are another must, as well as a proper clamping of the pedicle if a big haemorrhage is encountered, as means of clear and safe control. Another point is to always maintain great care with the use of electrosurgery. Under certain conditions, dissection of the structures is more hazardous (Fig. 2.10).
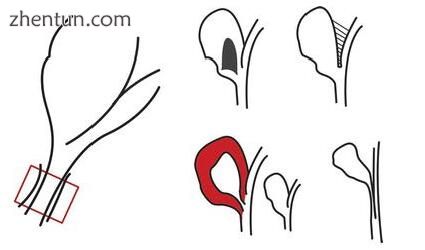
Fig. 2.10 Ideal dissection area and reasons for this dissection being more difficult: large stone in the infundibulum, extensive local adhesions, acute inflammation and anatomical anomalies
As principles to reduce the incidence, one can recommend:
Use of 30° optic.
Use of clear and proper methods for retract and expose to the surgical field.
Dissection of Calot’s triangle, starting close to the gallbladder.
Unequivocal identification of cystic duct and artery before they are divided:
Find the cystic duct by starting dissection at the triangle of Calot.
Clear the medial wall of infundibulum.
And trace the cystic duct on an uninterrupted line into the base of the gallbladder.
There are factors that may suggest that the structure being dissected is the CBD, instead of the cystic duct (> Ø duct, course behind duodenum, unexpected duct, large artery, etc.).
Some “principles” have been widely mentioned as rules to prevent lesions. But some may prove wrong: “Clearly identify the junction of the cystic duct and CBD”. Too much dissection work in here can lead to problems such as devascularisation with late strictures.
“Use routine IO cholangiography”. Although useful in many situations (confusing anatomy, difficult dissection, anomaly suspected), it brings another possible problem: there is a danger of misinterpretation, giving a false sense of security. The “tricks” the brain does before can also happen with cholangiography. And many lesions happen after cholangiography!
Facing some difficulties, there are options to deal with it: When a wide cystic duct is found, the surgeon may use 11-mm clips, if available, or use 9 mm at first (it will not close the whole lumen), followed by applying a premade endoloop knot.
If many adhesions are present, dissection must stick close to the gallbladder, and special care regarding electrosurgery has to be considered; minimise using monopolar diathermy as much as you can.
With a big stone in the Hartman pouch, there are ways to move it out of the way, simplifying dissection: try to move the stone up and grasp the Hartman below it.
Or use a lateral grasper for retracting the liver, without holding the fundus. The other two graspers manipulate the stone up. If this fails, try to support the Hartman by a grasper, and dissect the Calot’s triangle. Again, if this fails, open the Hartman pouch, and extract the stone.
When the left lobe of the liver encroaches the operative field, making visualisation difficult, raise the right shoulder of the patient, or use a long port or retractor from the epigastric incision. The surgeon can also retract the fundus upwards and medially. Finally, one may put a port more to retract the left lobe.
In some cases, the gallbladder is difficult to grasp; it is necessary to empty the GB totally or partially.
Anytime a surgeon considers that an anomaly may exist, one of three solutions shall be used:
Intraoperative cholangiography (properly interpreted) Getting a second opinion (presence of the help in the OT) Convert
2.4 Main Dissection Techniques
There are two main techniques to execute laparoscopic cholecystectomy: 1) The infundibular technique [14]. In this technique, the surgeon is taught to clear the infundibulum of the gallbladder (bowl of a funnel) down to the cystic duct (stem of the funnel) all the way around 360°.
Supposedly, when the funnel is seen, the cystic duct is identified.
2) The Critical View of Safety approach [15–17] which was mentioned before, and which is based on the fact that it is considered to have a safe and clear anatomy to finish surgery only when nothing else than two structures are visible coming out of the gallbladder. CVS (Critical View of Safety) is not really a dissection method; it is more a safety identification approach. It was first described in 1992 but only called as CVS in 1995 [15–17].
When approaching the gallbladder, it is necessary to remember that “biliary inflammation fusion” sticks anatomical elements together and makes it difficult to find where one structure starts and another ends. It makes the cystic duct look like the CBD and can change an “easy” cholecystectomy into a “difficult” one.
CVS has, as its true value, minimisation of risks. Using this approach, surgeon’s limit for conversion becomes lower or increases the possibility of using ancillary techniques like intraoperative cholangiography to better evaluate the picture, minimising risks (see Videos 2.1, 2.2 and 2.3).
Steven Strasberg [15, 18] is very critical of infundibular approach and considers it as an “error trap”, when trying to identify the cystic duct. His reasoning is that, the funnel shape, which is necessary to obtain the correct view, may, sometimes, be obtained by the dissection itself, and the stem of this funnel is not the cystic duct; this is because, in this technique, the surgeon is taught to clear the infundibulum of the gallbladder (bowl of a funnel) down to the cystic duct (stem of the funnel) all the way around 360°. Supposedly, when the funnel is seen, the cystic duct is identified. If the view is obtained by the dissection, the error is there, and another structure other than the cystic duct is cut.
The basis of CVS consists in three fundamental steps: no fibrotic tissue or fat at the Calot’s triangle, freeing the lower third of the gallbladder from its bed and checking the two structures (only two) coming into the gallbladder.
Finally, which suggestions and recommendations on measures to minimise the problem can be given?
Mainly two: following guidelines and improving training and education. Some guidelines are well established and have good grades of recommendation: optimal exposure to reach the Critical View of Safety is highly recommended
(GoR B). Although this can be achieved with the 0°, 30° or 45° optics, the CBD is more difficult to see with the 0° because it lies parallel to the scope. Rotation of the angled scopes provides different visualisation of the surgical field. This was already proposed long ago [16].
Inability to reach the Critical View of Safety and/or to identify the source and safely control bleeding, are indications for conversion (GoR A).
It is recommended to have supervised structured training, starting with skills courses (GoR B).
In some countries, it is mandatory to have a routine demonstration that CVS was obtained, either by photos or by video recording [16, 17].
Clearly, although BDI do occur in the hands of expert surgeons, inadequate experience is a risk factor.
New educational methods shall be put into practice, and already enough experience exists to understand this. Besides known exercises and properly structured courses, some more recent ideas have been understood. Expert surgeons can be identified, and their techniques have to be put in practice in teaching methods; they must share their practical preventing measures. This may bring learners faster to the level of “experts”.
Experts have more knowledge and, consequently, superior performance, although some of the reasons for this cannot be clearly understood; the most important is called “hidden knowledge”. This has three types:
Informal knowledge – from experience, but unwritten: does not exist in textbooks. An example is something many have experienced: the expert tells the resident to stop and look “here” or “there”. Looking, one finds that there was a reason for that. But all the expert can say is “It just didn’t look right”.
Impressionistic knowledge – experts are always, even unconsciously, looking back into “past experiences”. They have some “impressions” of some situations, with a “feeling of possible danger” in the presence of certain signs, not described.
Self-regulation knowledge – deep knowledge about themselves and about how they act.
Other evident but not so often followed principles – these can be generalised for any surgical approach – are the constant use of the highest human and surgical good sense, as well as keeping an adequate knowledge of the anatomy, and of the anomalies. Last, but by no means least, whenever in doubt, stop and re-evaluate; one will be surprised by the number of times this will change the
options and attitudes. And always keep a humble position; be aware of the situations and of the capacities, human and technical, existing. Every time it feels advisable, do not hesitate to ask for help.
As general conclusions, it can be said that these are serious lesions. They can be avoided (or at least, minimised), by a cautious approach, a surgeon’s liberal policy of conversion and asking for specialised help when facing unexpected intraoperative problems. No surgeon is “protected” against this problem, and correct training in laparoscopy is mandatory. These lesions, by their specificity, should always be dealt with by experienced teams in reference centres. Only this way, complications can be minimised and quality and good outcomes guaranteed.
参考:Complications in Laparoscopic Surgery A Guide to Prevention and Management |