|
Cryptic tonsils immediately following surgical removal (bilateral tonsillectomy).

手术摘除后立即隐藏扁桃体(双侧扁桃体切除术)。
扁桃体切除术是一种外科手术,其中扁桃体(以下称“扁桃体”)从咽侧称为扁桃体窝的凹陷处被去除。该过程是针对急性扁桃体炎的重复发生,阻塞性睡眠呼吸暂停的睡眠手术,鼻气道阻塞,白喉载体状态,打鼾或扁桃体周围脓肿而进行的。对于儿童,扁桃体切除术通常与腺样体切除术相结合,腺样体切除术是去除腺样体(也称为“咽扁桃体”或“鼻咽扁桃体”)。这两种方法的组合被称为“腺样体切除术”或“T&A”。腺样体切除术在成人中并不常见,其中腺样体比儿童小得多,并且很少引起问题。虽然目前的扁桃体切除手术比20世纪50年代到70年代的手术频率要低得多,但它仍然是美国和其他许多西方国家儿童常见的手术方法。然而,扁桃体切除术仍然是一个有争议的手术,因为它的益处在大多数情况下似乎只是适度和暂时的,已经认识到与手术相关的危害,并且有几种迹象表明扁桃体切除术可能长期损害免疫系统,特别是在进行在年轻的时候。
内容
1个历史
2医疗用途
2.1有效性
2.2扁桃体切除术的过度治疗
3手术过程
3.1方法
4术后护理
5个并发症
6对免疫系统的影响
7图片库
8参考
历史
扁桃体切除术已进行了两千多年,几个世纪以来受到不同的欢迎[1]。该程序在一些书中被称为约1000年前的“印度医学”(非证据文献)。其他人则称之为用食指指甲清洁扁桃体。大约一千年后,罗马贵族Aulus Cornelius Celsus(公元前25年 - 公元50年)描述了一种使用手指(或必要时使用钝钩)的手术方法,扁桃体在切割前与邻近组织分离[1]。 Galen(121-200 CE)率先倡导使用被称为圈套的外科手术器械,在Aetius(490 CE)建议部分切除扁桃体之前,这种做法一直很普遍,他写道:“那些剔除整个器官的人扁桃体可以同时清除完全健康的结构,从而导致严重的出血“。[1]在7世纪,Paulus Aegineta(625-690)描述了扁桃体切除术的详细程序,包括处理不可避免的手术后出血。在这个过程之前已经有1200年的历史了,并且具有如此精确和细节。[1]
中世纪的人看到扁桃体切除术变得不受欢迎; Ambroise Pare(1509)写道,这是“一个不好的操作”,并提出一个程序,其中包括用绷带逐渐勒死。这种方法由于其引起的巨大疼痛和通常伴随的感染而不受患者欢迎。苏格兰医师Peter Lowe在1600年总结了当时使用的三种方法,包括圈套,结扎和切除术。[1]当时,扁桃体的功能被认为是鼻子分泌物的吸收;假定去除大量的扁桃体组织会干扰清除这些分泌物的能力,导致它们积聚在喉中,导致声音嘶哑。出于这个原因,像迪奥尼斯(1672)和洛伦茨海斯特(Lorenz Heister)这样的医生对这一程序进行了指责。
Tonsil guillotine.

扁桃体铲除刀。
1828年,医生Philip Syng Physick修改了本杰明·贝尔最初设计的用于去除悬雍垂的现有器械; 该器械被称为扁桃体铲除刀(后来被称为扁桃体切除器),已成为扁桃体切除标准器械80多年的历史[1]。 到1897年,在美国医生Ballenger指出在大部分病例中部分切除未能完全缓解症状后,进行完全而非部分切除扁桃体变得更为常见。 他的研究结果使用了一种包括用手术刀和镊子去除扁桃体的技术,比部分去除好得多; 使用断头台的扁桃体切除术最终在美国失宠。[1]
医疗用途
3 days post tonsillectomy

扁桃体切除术后3天
当患者经历急性扁桃体炎的复发性感染时,可以指示扁桃体切除术。由于扁桃体大小在3岁时达到最大值,然后逐渐消退,扁桃体切除术通常会延迟,除非感染频率绝对必要。促使扁桃体切除术的数量随着发作的严重程度而变化。一例,即使是严重的,通常还不足以让大多数外科医生决定是否需要扁桃体切除术。 1983年的天堂定义复发性扁桃体炎保证手术的发作频率标准为
一年七个或更多,两年每年五个或更多,或三年每年三个或更多。这些是扁桃体切除术的绝对适应症。[2]
根据美国耳鼻喉科和头颈外科学会(AAO-HNS)2012年的指南,扁桃体切除术指示如下:
临床医生可能会推荐扁桃体切除术治疗喉癌复发,过去一年至少有7次发作,或者每年至少5次发作2年,或者每年至少发作3次,持续3年,并在每次发作时记录病历喉咙痛和以下一种或多种情况:体温> 38.3°C,腺病,扁桃体分泌物或A组β-溶血性链球菌阳性试验[3]
扁桃体切除术有时也用于对扁桃体长期遭受痛苦的患者[4]。
最近,美国耳鼻咽喉 - 头颈外科基金会发表了临床实践指南[5] [6]。专家组强烈建议:
如果过去一年少于7次发作,或过去2年每年发作少于5次,或在过去3年每年发作少于3次,注意等待复发性喉咙感染;
评估不符合声明2中标准的复发性喉部感染患儿,以修改可能有利于扁桃体切除术的因素,这些因素可能包括但不限于多种抗生素过敏/不耐受,周期性发热,口疮性口炎,咽炎和腺炎或病史扁桃体周围脓肿;
询问患有睡眠呼吸障碍和扁桃体肥大的儿童,看看可能改善扁桃体切除术后的并发症,包括发育迟缓,学习成绩差,遗尿和行为问题;
咨询有关扁桃体切除术的护理人员作为改善多导睡眠监测异常的儿童健康的手段,他们也患有扁桃体肥大和睡眠呼吸紊乱;
辅导照顾者睡眠呼吸障碍可能在扁桃体切除术后持续或复发,并可能需要进一步管理;
倡导扁桃体切除术后的疼痛管理并教育护理人员了解疼痛管理和重新评估的重要性;和
执行扁桃体切除术的临床医生应至少每年确定一次和二次扁桃体切除术后出血的发生率。
效用
科学证据表明,扁桃体切除术对于减少喉咙痛的频率和严重程度只有适度的效果,并且完全没有排除喉咙痛,可能是因为大多数喉咙痛不是由感染的扁桃体引起的[7] [8] [9 ] [10] [11] [12]由于儿童通常会出现扁桃体相关疾病,因此手术后好处也只会持续一到两年。[13] [14]一些患者确实经历了长期的结果,但需要做更多的信息和研究来描绘关于此问题的全貌。[15]
这引发了一些问题,即哪些儿童受益足以证明进行该手术的合理性。[16]即使在符合严格标准的儿童中,他们受到喉咙痛的严重影响,证据表明只有短期益处。[17]如果没有扁桃体切除术,符合这些严格标准的儿童在未来两年内可能会有6个喉咙痛,而接受手术的患者在未来两年内可能会有3个喉咙痛。两年后,无论孩子是否接受手术,喉咙痛频率差异不大[14]。患有无证喉咙痛或喉咙痛的儿童在接下来的几年中似乎没有多少喉咙痛,因此扁桃体切除术不值得。[9] [18]
严格的标准是,儿童应该经历: - 前一年记录的7例喉咙痛 - 前两年每年5例 - 前三年每年3例,喉咙痛应包括记录的肿大的淋巴腺或升高的温度,或咽拭子阳性(显示链球菌感染)或扁桃体上见到的脓。
“喉咙痛”一词比咽喉感染或扁桃体炎更受欢迎,因为如果不进行咽喉拭子,医生不能可靠地区分感染引起的喉咙痛和其他原因引起的喉咙痛。此外,同一名患者可能被另一名患者描述为患有“扁桃体炎”或“喉咙痛”,因此使用一项而不是另一项取决于医生和患者,这使得其成为不可靠的理由手术。
许多扁桃体切除术也用于睡眠呼吸暂停,但这没有充分的证据表明这是否比手术更有效[9] [19]。由于不知道扁桃体切除术对呼吸相关问题的有效性,因此目前正在进行临床试验来调查是否有效。 (小儿腺样体切除术用于打鼾(PATS)),(小儿OSA手术的随机对照试验)
用扁桃体切除术进行过度治疗
不同国家之间和国家之间的扁桃体切除率存在显著差异,这表明许多扁桃体切除术实际上可能没有充分的医学证明。[9] [20] (达特茅斯卫生保健地图集,每1000名儿童的扁桃体切除术)2015年,比利时,芬兰和挪威的扁桃体切除率是英国的两倍,但西班牙,意大利和波兰的比率至少降低了四分之一。 (Eurostat)美国的儿童扁桃体切除术率是英国的三倍,是世界上最高的。[9] [21]
2010年的一项研究发现,在2000年至2005年间,英格兰最高的地区性年度扁桃体切除率为754/100000,是平均每100.000 304的两倍多,是每100.000 102的最低值的七倍。 [22] 2006年,首席医官利亚姆唐纳森透露,不必要的扁桃体切除术和不必要的子宫切除术加起来每年花费英国国家卫生服务机构2100万英镑[23]。
耳鼻喉科外科医生摘除扁桃体的原因很复杂,包括临床医生和患者对有效性的信念。财政激励和家长压力也被认为是起作用的。[24] [25] [26] [27] [28]但是,随机对照试验的科学证据不足以支持使用扁桃体切除术治疗复发性喉咙痛的阻塞性睡眠呼吸暂停,除非其符合上述标准。有证据表明扁桃体切除术会给患者带来短期和长期的风险。英国有证据表明,接受扁桃体切除术的大多数儿童并未接受手术,其中中等程度的扁桃体切除率较高(低于美国,德国,挪威,比利时,高于西班牙或意大利)[29]。即使孩子确实有益,那么这些好处是否证明了与扁桃体切除术有关的短期和长期风险仍然值得怀疑。
然而,在过去的几十年中,扁桃体切除术已经不那么常见了,因为人们意识到警戒等待通常比手术更好,因为随着年龄的增长投诉往往自发地消退。此外,越来越多的医生认为扁桃体作为第一道防线在人体免疫系统中扮演着重要的角色,即使不是非常重要的角色。
外科手术
至少在过去的50年里,扁桃体切除术是通过从周围的筋膜,即所谓的“全面”或囊外扁桃体切除术中解剖出扁桃体来实现的。包括疼痛和出血在内的问题导致近期60-100年前流行的小儿扁桃体切除术或“扁桃体切开术”的兴趣重新抬头,以努力减少这些并发症[30]。普遍接受的“全面”扁桃体切除手术使用手术刀和钝器解剖或电刀,尽管也使用了谐波手术刀或激光。通过电灼,缝线结扎和局部使用凝血酶(一种诱导血液凝固的蛋白质)停止出血。
重要的主要问题在于阻塞性睡眠呼吸暂停中次全切除扁桃体切除术的益处是否持久。目前还没有关于扁桃体切除术对睡眠呼吸暂停长期有效性的随机对照试验。[9] [19]
方法
手术刀是许多耳鼻喉专家的首选手术器械。但是,还有其他技术和每个简要的评论如下:
解剖和圈套法:使用镊子和剪刀,用称为“圈套”的线圈去除扁桃体,以前是耳鼻喉科医师最常用的方法,但在很大程度上取代了其他技术。[需要的引证]该程序要求患者进行全身麻醉;扁桃体被完全去除并且剩余的组织表面被烧灼。患者将以最小的术后出血离开。
电烙术:电烙术使用电能来分离扁桃体组织,并通过烧灼帮助减少失血。研究表明,电灼的热量(400°C)可能导致周围组织的热损伤。这可能会在术后期间造成更多不适。
射频消融:单极射频热消融通过插入扁桃体的探头将射频能量传递至扁桃体组织。该程序可以在轻度镇静或局部麻醉下的办公室(门诊)中进行。治疗后,扁桃体内发生疤痕,导致其在几周内缩小。治疗可以进行多次。这种技术的优点是最小的不适,易于操作,并立即返回工作或学校。手术后留下扁桃体组织,但不显著。建议这种手术治疗扁桃体肿大,而不是慢性或复发性扁桃体炎。
扁桃体切除术:使用血浆去除扁桃体进行外科手术。 Coblation技术结合了射频能量和盐水来创建等离子体场。等离子体场能够解离目标组织的分子键,同时保持相对较低的温度(40-70°C)[31],从而对周围健康组织造成最小或无损伤。 Cobalt扁桃体切除术在手术室内进行,病人处于全身麻醉状态。扁桃体切除术通常有两个主要原因:扁桃体肥大(扁桃体肥大)和扁桃体炎复发。据称这种技术可以减少疼痛,加快愈合速度,减少术后护理。[32]然而,对21项研究的回顾提出了关于疼痛程度的相互矛盾的结果,其相对安全性尚未得到证实[33]。这种技术被批评为高于预期的出血率,可能是由于低温可能不足以密封分开的血管,但几篇论文提供了相互矛盾的(一些积极的,一些消极的)结果。最近有关扁桃体切除术的研究表明,疼痛和怀旧减少;术中或术后并发症少[35];延迟出血的发生率较低,在儿童人群中更为显着,[36] [37] [38]恢复日常活动,减少扁桃体床的继发感染,明显降低继发性出血的发生率[39]。与电外科手术不同,Coblation扁桃体切除术在接触的组织上产生明显较低的温度[40]。长期的研究似乎表明,外科医生对该技术的经验并不多。
谐波手术刀:这种医疗设备使用超声波能量以55kHz振动其刀片。肉眼看不见,振动将能量传递给组织,同时提供切割和凝固。周围组织的温度达到80°C。该程序的支持者声称,最终结果是精确切割,热损伤最小。
热焊接:一种使用纯热能密封和分开组织的新技术。没有热传播意味着周围组织的温度仅比正常体温高2-3℃。临床报告显示术后疼痛最小(不需要麻醉止痛药),无水肿(肿胀),几乎没有出血发生。美国的医院将这一程序称为“无痛扁桃体切除术”。也称为组织焊接。
二氧化碳激光:当使用激光进行扁桃体切除术时,这被称为激光辅助系列扁桃体切除术(LAST)。[41]这与使用激光来减少或重新表面扁桃体的程序不同(例如激光密码分解)。如果缺乏某些禁忌症例如敏感性胃肠反射,LAST可以在局部麻醉下作为门诊手术进行。通常使用二氧化碳激光器,并扫描每个扁桃体8-10次。烟雾从嘴里吸出来防止吸入烟雾。通常需要多个程序,每个程序大约需要20分钟。 LAST后的疼痛可能比其他扁桃体切除术方法更大。由于多次会议的频繁需求,这种治疗可能会比单一疗程扁桃体更昂贵。
术后护理
手术后大约两周,喉咙痛会持续,而手术后的疼痛是显著的,可能需要住院治疗[42]。恢复可能需要7至10天,在此期间适当的补水非常重要,因为脱水会增加喉部疼痛,导致流体摄入不良的恶性循环[43] [44]。
在某些时候,最常见的情况是术后7-11天(但偶尔会持续两周(14天)),当痂从手术部位脱落时会出现出血。总体出血风险约为1-2%。成年人尤其如此,尤其是70岁以上的男性,并且在手术当天出现四分之三的出血事件[45]。大约3%的成人患者此时会出现严重出血,有时可能需要手术治疗。
手术后疼痛缓解可能会有所改变。传统上,相对温和的麻醉性镇痛药如含可待因的对乙酰氨基酚,用于缓和疼痛以及用于更严重疼痛的更强的麻醉性镇痛药提供了疼痛缓解。最近(2011年1月),由于担心对乙酰氨基酚组分的肝脏毒性,FDA减少了推荐的24小时总剂量。另一种方法是使用非甾体抗炎药,这些药物本身引起人们担心它们对血小板的影响可能会增加术后出血的风险[46]。反过来,这又重新对传统的“囊外切除术”以外的技术产生兴趣,希望手术后的疼痛可能会减少[47]。
扁桃体切除术似乎在成人中比儿童更痛苦,尽管在应答方面会有个体差异[48]。
并发症
虽然扁桃体切除术是一种相对安全的手术,但有时会发生严重的并发症(特别是出血,脱水和感染)和死亡[9] [49] [50]。轻微的并发症包括语音变化和味觉障碍。[51] [52] [53]由于术后出血,与扁桃体切除术有关的发病率为2%至4%在美国,3.6%的儿童在扁桃体切除术后重新入院,主要是因为脱水或出血。 [9] [54]由于出血,气道阻塞或麻醉并发症,死亡率为15,000。
在手术期间可以给予单剂量的皮质类固醇药物地塞米松以防止手术后呕吐[56]。一项系统评价发现,手术过程中一剂地塞米松可以防止每五名接受该药物的儿童中有一名患儿出现呕吐[56]。审查还发现,这些儿童更快速地恢复正常饮食,手术后疼痛更少[56]。
最近的一项研究表明,年幼儿童(0〜7岁)的扁桃体切除术与手术后几年的体重增加相关[57]。但是,没有确定因果关系。[58]
对免疫系统的影响
扁桃体切除术是否对免疫系统产生负面影响仍存在争议。然而,多项研究证实了以前的扁桃体切除术史和多种疾病之间的相关性,例如:
霍奇金病[59] [60] [61] [62]
非霍奇金淋巴瘤[63]
喉癌[64]
食管癌[65]
甲状腺癌[66] [67]
乳腺癌[68] [69] [70]
前列腺癌[71]
舌癌的基础[72]
白血病[73][74][75][76]
哮喘[77][78]
干草热[79] [80]
流感[78]
肺部感染[78]
肾脏感染[78]
肠易激综合征[81]
克罗恩病[82] [83] [84] [85] [86]
阑尾炎[87]
心脏病发作[88]
结节病[89]
类风湿性关节炎[90] [91]
咽后壁和咽旁脓肿[92]
中耳炎[78] [93]
多发性硬化症[94] [95] [96] [97]
深颈部感染[98]
脊髓灰质炎[99][100][101][102]
复发性蜂窝组织炎[103]
原发性胆道胆管炎[104] [105]
鼻窦炎[78][106]
与链球菌感染相关的小儿自身免疫性神经精神障碍[107]
此外,其他研究发现扁桃体切除术可能导致:
血清免疫球蛋白水平降低[108]
分泌性免疫球蛋白A水平永久降低[108] [109] [110]
免疫球蛋白G3水平永久降低[111]
自身免疫性疾病的风险增加[78] [112]
18岁至44岁之间的死亡率增加[113]
慢性疾病的风险增加[114]
总体癌症风险增加[67] [70]
呼吸系统疾病风险增加2至3倍[78]
传染病的风险增加[78]
过敏风险增加[78]
图片库
Throat with tonsilloliths.

喉咙与扁桃体。
Bilateral Tonsillectomy—Cryptic Tonsils
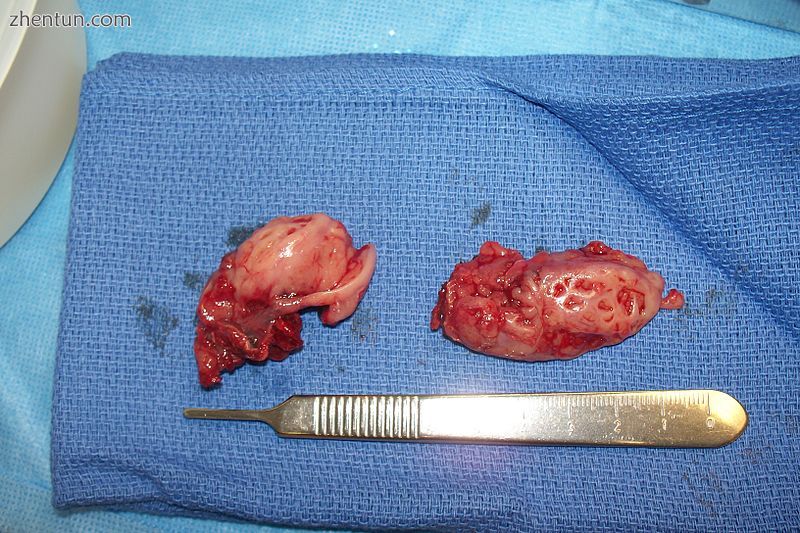
双侧扁桃体切除隐匿扁桃体
Two removed tonsils.
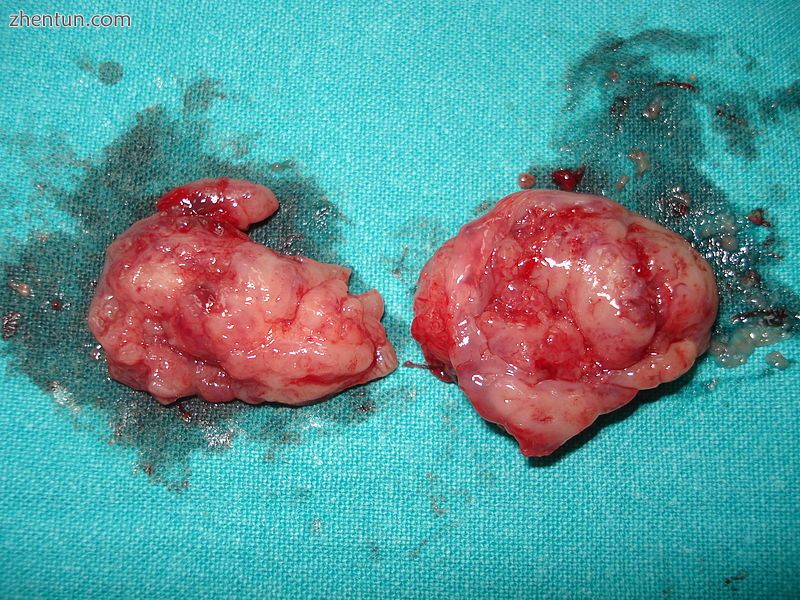
两个扁桃体切除。
Throat 1 day after a tonsillectomy.

扁桃体切除术后1天咽喉。
Throat some days after a tonsillectomy.

扁桃体切除术后几天咽喉。
参考:
1. McNeill RA., RA (1 June 1960). "A History of Tonsillectomy: Two Millenia of Trauma, Hæmorrhage and Controversy". Ulster Medical Journal. 29 (1): 59–63. PMC 2384338 Freely accessible. PMID 20476427.
2. Paradise JL (1983). "Tonsillectomy and Adenoidectomy" (PDF). II IAPO/IFOS Pediatric ENT Manual. pp. 122–26.
3. American Academy of Otolaryngology – Head and Neck Surgery. 2012 Clinical Indicators Compendium. Clinical Indicators: Tonsillectomy, Adenoidectomy, Adenotonillectomy.
4. Svoboda, Elizabeth (31 August 2009). "In Tonsils, a Problem the Size of a Pea". The New York Times. Retrieved 8 January 2011.
5. Baugh RF, Archer SM, Mitchell RB, Rosenfeld RM, Amin R, Burns JJ, Darrow DH, Giordano T, Litman RS, Li KK, Mannix ME, Schwartz RH, Setzen G, Wald ER, Wall E, Sandberg G, Patel MM (January 2011). "Clinical practice guideline: tonsillectomy in children". Otolaryngology–Head and Neck Surgery. 144 (1 Suppl): S1–30. doi:10.1177/0194599810389949. PMID 21493257.
6. Randel, A (1 September 2011). "AAO-HNS Guidelines for Tonsillectomy in Children and Adolescents". American Family Physician. 84 (5): 566–73. PMID 21888309.
7. Blakley, BW; Magit, AE (2009). "Response to: The role of tonsillectomy in reducing recurrent pharyngitis: A systematic review, from Jeremy Hornibrook". Otolaryngology–Head and Neck Surgery. 141 (1): 155–56. doi:10.1016/j.otohns.2009.04.017.
8. Blakley, BW; Magit, AE (March 2009). "The role of tonsillectomy in reducing recurrent pharyngitis: a systematic review". Otolaryngology–Head and Neck Surgery. 140 (3): 291–97. doi:10.1016/j.otohns.2008.12.013. PMID 19248931.
9. Burton, Martin J.; Glasziou, Paul P.; Chong, Lee Yee; Venekamp, Roderick P. (2014-01-01). "Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis". Cochrane Database of Systematic Reviews. 11: CD001802. doi:10.1002/14651858.CD001802.pub3. ISSN 1469-493X. PMID 25407135.
10. Staaij, B. K. van; Akker, E. H. van den; Heijden, G. J. M. G. van der; Schilder, A. G.; Hoes, A. W. (2005-01-01). "Adenotonsillectomy for upper respiratory infections: evidence based?". Archives of Disease in Childhood. 90 (1): 19–25. doi:10.1136/adc.2003.047530. ISSN 0003-9888. PMC 1720065 Freely accessible. PMID 15613505.
11. Fry, John (1957-01-19). "Are All "T's and A's" Really Necessary?". The BMJ. 1 (5011): 124–29. doi:10.1136/bmj.1.5011.124. ISSN 0007-1447. PMC 1974118 Freely accessible. PMID 13383209.
12. Staaij, Birgit K. van; Akker, Emma H. van den; Rovers, Maroeska M.; Hordijk, Gerrit Jan; Hoes, Arno W.; Schilder, Anne G. M. (2004-09-16). "Effectiveness of adenotonsillectomy in children with mild symptoms of throat infections or adenotonsillar hypertrophy: open, randomised controlled trial". The BMJ. 329 (7467): 651. doi:10.1136/bmj.38210.827917.7C. ISSN 0959-8138. PMC 517640 Freely accessible. PMID 15361407.
13. Morad, A; Sathe, NA; Francis, DO; McPheeters, ML; Chinnadurai, S (February 2017). "Tonsillectomy Versus Watchful Waiting for Recurrent Throat Infection: A Systematic Review". Pediatrics. 139 (2): e20163490. doi:10.1542/peds.2016-3490. PMC 5260157 Freely accessible. PMID 28096515.
14. Marshall, Tom (2002-12-01). "Effectiveness of tonsillectomy? A reply to Howel et al". Family Practice. 19 (6): 707–708. doi:10.1093/fampra/19.6.707-a. ISSN 0263-2136.
15. Burton MJ, Glasziou PP, Chong LY, Venekamp RP (2014). "Surgical removal of the tonsils (tonsillectomy) for chronic or recurrent acute tonsillitis | Cochrane". Cochrane Database Syst Rev (11): CD001802. doi:10.1002/14651858.CD001802.pub3. PMID 25407135.
16. Goodman, David C.; Challener, Greg J. (2012-05-01). "Tonsillectomy: A Procedure in Search of Evidence". The Journal of Pediatrics. 160 (5): 716–718. doi:10.1016/j.jpeds.2012.01.033. ISSN 0022-3476.
17. Marshall T (1998). "A review of tonsillectomy for recurrent throat infection" (PDF). British Journal of General Practice. 48 (431): 1331–35. PMC 1410132 Freely accessible. PMID 9747553.
18. Paradise JL, et al. (2002). "Tonsillectomy and adenotonsillectomy for recurrent throat infection in moderately affected children". Pediatrics. 110 (1): 7–15. doi:10.1542/peds.110.1.7. PMID 12093941.
19. Venekamp RP, et al. (2015). "Tonsillectomy or adenotonsillectomy versus non-surgical management for obstructive sleep-disordered breathing in children". Cochrane Database of Systematic Reviews (10). |article= ignored (help)
20. McPherson K, et al. (1982). "Small-Area Variations in the Use of Common Surgical Procedures: An International Comparison of New England, England, and Norway". New England Journal of Medicine. 307: 1310–1314. doi:10.1056/NEJM198211183072104.
21. Baigh RF, et al. (2011). "American Academy of Otolaryngology-Head and Neck Surgery Foundation. Clinical practice guideline: tonsillectomy in children". Otolaryngol Head Neck Surg. 144: S1–30. doi:10.1177/0194599810389949.
22. Suleman, M.; Clark, M. P. A.; Goldacre, M.; Burton, M. (April 2010). "Exploring the variation in paediatric tonsillectomy rates between English regions: a 5-year NHS and independent sector data analysis". Clinical otolaryngology: official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 35 (2): 111–117. doi:10.1111/j.1749-4486.2010.02086.x. ISSN 1749-4486. PMID 20500580.
23. "Billions of NHS money wasted on 'ineffective' operations". Evening Standard. Retrieved 2018-01-27.
24. "Dr. Obama's Tonsillectomy". Wall Street Journal. 2009-07-27. ISSN 0099-9660. Retrieved 2017-10-18.
25. Bolande, Robert P. (1969-03-13). "Ritualistic Surgery — Circumcision and Tonsillectomy". New England Journal of Medicine. 280 (11): 591–596. doi:10.1056/NEJM196903132801105. ISSN 0028-4793. PMID 4885060.
26. Furman Robert A (1959-02-01). "Handling parental pressure for T and A". The Journal of Pediatrics. 54 (2): 195–199. doi:10.1016/S0022-3476(59)80062-7. ISSN 0022-3476.
27. Burton, M. J (2008-02-01). "Commentary: Tonsillectomy--then and now". International Journal of Epidemiology. 37 (1): 23–25. doi:10.1093/ije/dym259. ISSN 0300-5771.
28. Berger, R. (September 1976). "The question of tonsillectomy and adenoidectomy: still with us in 1976". The Journal of the American Osteopathic Association. 76 (1): 32–34. ISSN 0098-6151. PMID 1048964.
29. Marshall T, et al. (2001). "How many tonsillectomies are evidence-based?". Journal of Clinical Excellence. 3 (1): 23–25.
30. Walton J, Ebner Y, Stewart MG, April MM (2012). "Systematic Review of Randomized Controlled Trials Comparing Intracapsular Tonsillectomy With Total Tonsillectomy in a Pediatric Population". Archives of Otolaryngology—Head & Neck Surgery. 138 (3): 243–49. doi:10.1001/archoto.2012.16. PMID 22431869.
31. "COBLATION Plasma Technology - ENT". Smith & Nephew US Professional. Retrieved 15 July 2016.
32. Friedman M, LoSavio P, Ibrahim H, Ramakrishnan V (2003). "Radiofrequency tonsil reduction: safety, morbidity, and efficacy". The Laryngoscope. 113 (5): 882–7. doi:10.1097/00005537-200305000-00020. PMID 12792327.
33. Windfuhr JP. (2007). "[Coblation tonsillectomy: a review of the literature.]". HNO. 55 (5): 337–48. doi:10.1007/s00106-006-1523-3. PMID 17431570.
34. Sun-Moon, Hong (June 14, 2013). "Coblation vs. Electrocautery Tonsillectomy: A Prospective Randomized Study Comparing Clinical Outcomes in Adolescents and Adults". Clinical and Experimental Otorhinolaryngology. 6 (2): 90. doi:10.3342/ceo.2013.6.2.90.
35. Omrani, M (January 2012). "Coblation versus traditional tonsillectomy: A double blind randomized controlled trial". Journal of Research in Medical Sciences. Isfahan University of Medical Sciences. 17 (1): 45–50. PMC 3523437 Freely accessible. PMID 23248656.
36. Walner, DL (October 1, 2012). "Coblation tonsillectomy in children: incidence of bleeding". The Laryngoscope. 122 (10): 2330–6. doi:10.1002/lary.23526. PMID 22833366.
37. Kahn, I (February 4, 2012). "Coblation tonsillectomy: is it inherently bloody?". European Archives of Oto-Rhino-Laryngology. 269 (2): 579–83. doi:10.1007/s00405-011-1609-8. PMID 21547390.
38. Mosges, R (June 5, 2011). "Hemorrhage rate after coblation tonsillectomy: a meta-analysis of published trials". European Archives of Oto-Rhino-Laryngology. 268 (6): 807–16. doi:10.1007/s00405-011-1535-9. PMC 3087106 Freely accessible. PMID 21373898.
39. Beloso, A (November 2003). "Coblation tonsillectomy versus dissection tonsillectomy: postoperative hemorrhage". The Laryngoscope. 113 (11): 2010–2013. doi:10.1097/00005537-200311000-00029.
40. "COBLATION Tonsillectomy - My Tonsils". My Tonsils.com. Retrieved 11 July 2016.
41. "Interventional procedure overview of laser assisted serial tonsillectomy" (PDF). National institute of clinical excellence. Retrieved 30 November 2013.
42. Graham, John M.; Glenis K. Scadding; Peter D. Bull (2008). Pediatric ENT. Springer. p. 136. ISBN 3-540-69930-9.
43. Timby, Barbara Kuhn; Nancy Ellen Smith (2006). Introductory medical-surgical nursing. Lippincott Williams & Wilkins. p. 357. ISBN 0-7817-8032-2.
44. Pemberton, Cecilia M. (1988). Mayo Clinic diet manual. B.C. Decker. ISBN 1-55664-032-3.
45. Windfuhr JP, Chen YS, Remmert S (2005). "Hemorrhage following tonsillectomy and adenoidectomy in 15,218 patients". Otolaryngology–Head and Neck Surgery. 132 (2): 281–86. doi:10.1016/j.otohns.2004.09.007. PMID 15692542.
46. Møiniche S, Rømsing J, Dahl JB, Tramèr MR (January 2003). "Nonsteroidal antiinflammatory drugs and the risk of operative site bleeding after tonsillectomy: a quantitative systematic review". Anesthesia & Analgesia. 96 (1): 68–77. doi:10.1213/00000539-200301000-00015. PMID 12505926.
47. Chimona T, Proimos E, Mamoulakis C, Tzanakakis M, Skoulakis CE, Papadakis CE (September 2008). "comparison of cold knife tonsillectomy, radiofrequency excision and thermal welding tonsillectomy in children". International Journal of Pediatric Otorhinolaryngology. 72 (9): 1431–6. doi:10.1016/j.ijporl.2008.06.006. PMID 18620759.
48. Graumüller S, Laudien B (November 2003). Postoperative pain after tonsillectomy—comparison of children and adults. Advances in Pediatric ORL. Proceedings of the 8th International Congress of Pediatric Otorhinolaryngology. 1254. Elsevier. pp. 469–72. doi:10.1016/S0531-5131(03)01073-2.
49. Coté CJ, et al. (2014). "Death or neurologic injury after tonsillectomy in children with a focus on obstructive sleep apnea: Houston, we have a problem!". Anesth Analg. 118: 1276–83. doi:10.1213/ANE.0b013e318294fc47.
50. Randall, David A.; Hoffer, Michael E. (1998-01-01). "Complications of Tonsillectomy and Adenoidectomy". Otolaryngology-Head and Neck Surgery. 118 (1): 61–68. doi:10.1016/S0194-5998(98)70376-6. ISSN 0194-5998.
51. Ilk, Hakki Gökhan; Eroğul, Osman; Satar, Bülent; Özkaptan, Yalçin (2002-12-01). "Effects of Tonsillectomy on Speech Spectrum". Journal of Voice. 16 (4): 580–586. doi:10.1016/S0892-1997(02)00133-9. ISSN 0892-1997.
52. Tomofuji, Seiichi; Sakagami, Masafumi; Kushida, Kyoko; Terada, Tomonori; Mori, Hiroshi; Kakibuchi, Masao (2005-12-01). "Taste disturbance after tonsillectomy and laryngomicrosurgery". Auris Nasus Larynx. 32 (4): 381–386. doi:10.1016/j.anl.2005.05.005. ISSN 0385-8146.
53. Tomita, Hiroshi; Ohtuka, Kenji (8 July 2009). "Taste Disturbance After Tonsillectomy". Acta Oto-Laryngologica. 122: 164–172. doi:10.1080/00016480260046571.
54. Johnson RF, et al. (2018). "Nationwide readmissions after tonsillectomy among pediatric patients - United States". International Journal of Pediatric Otorhinolaryngology. 107: 10–13. doi:10.1016/j.ijporl.2018.01.026.
55. Lee KL, p. 544.
56. Steward, DL; Grisel, J; Meinzen-Derr, J (10 August 2011). Steward, David L, ed. "Steroids for improving recovery following tonsillectomy in children". Cochrane Database of Systematic Reviews (8): CD003997. doi:10.1002/14651858.CD003997.pub2. PMID 21833946.
57. Wijga, AH; Scholtens, S; Wieringa, MH; Kerkhof, M; Gerritsen, J; Brunekreef, B; Smit, HA (Apr 2009). "Adenotonsillectomy and the development of overweight". Pediatrics. 123 (4): 1095–101. doi:10.1542/peds.2008-1502. PMID 19336367.
58. Wei, JL (Jun 2011). "Weight gain after tonsillectomy: myth or reality? Interpreting research responsibly". Otolaryngology–Head and Neck Surgery. 144 (6): 855–7. doi:10.1177/0194599811406674. PMID 21515804.
59. Liaw, K. L.; Adami, J.; Gridley, G.; Nyren, O.; Linet, M. S. (1997-09-04). "Risk of Hodgkin's disease subsequent to tonsillectomy: a population-based cohort study in Sweden". International Journal of Cancer. 72 (5): 711–713. doi:10.1002/(sici)1097-0215(19970904)72:5<711::aid-ijc1>3.0.co;2-v. ISSN 0020-7136. PMID 9311582.
60. Vianna, NicholasJ.; Greenwald, Peter; Davies, J.N.P. (1971). "TONSILLECTOMY AND HODGKIN'S DISEASE: THE LYMPHOID TISSUE BARRIER". The Lancet. 297 (7696): 431–432. doi:10.1016/s0140-6736(71)92416-0.
61. Vianna, NicholasJ; Davies, JackN P.; Harris, Steve; Lawrence, CharlesE; Arbuckle, Jeffrey; Marani, William; Wilkinson, John (1980-08-16). "TONSILLECTOMY AND CHILDHOOD HODGKIN'S DISEASE". The Lancet. 316 (8190): 338–340. doi:10.1016/S0140-6736(80)90339-6. ISSN 0140-6736.
62. KIRCHHOFF, LOUIS V.; EVANS, ALFRED S.; MCCLELLAND, KAREN E.; CARVALHO, RENATO P. S.; PANNUTI, CLAUDIO S. (1980-11-01). "A CASE-CONTROL STUDY OF HODGKIN'S DISEASE IN BRAZIL". American Journal of Epidemiology. 112 (5): 595–608. doi:10.1093/oxfordjournals.aje.a113032. ISSN 0002-9262.
63. Wang, Jun; Mack, Thomas M.; Hwang, Amie; Nathwani, Bharat N.; Hamilton, Ann; Cozen, Wendy (2011-11-18). "Innmune-Related Risk Factors for Non-Hodgkin Lymphoma in Twins". Blood. 118 (21): 1588–1588. ISSN 0006-4971.
64. Sokic, Slobodanka I.; Adanja, Benko J.; Marinkovic, Jelena P.; Vlajinac, Hristina D. (1995). "Risk factors for laryngeal cancer". European Journal of Epidemiology. 11 (4): 431–433. doi:10.1007/BF01721228. ISSN 0393-2990.
65. Garman, Katherine S.; Boutte, Harold J.; Furstenberg, Richard J. von; Chiu, Shih-Ting; Lloyd, Benjamin; Zhang, Cecelia; Onaitis, Mark; Chow, Shein-Chung; McCall, Shannon J. (2016). "Tu1179 Previous Tonsillectomy Is Associated With Increased Risk of Esophageal Cancer". Gastroenterology. 150 (4): S856. doi:10.1016/s0016-5085(16)32889-x.
66. Bross, Irwin D. J. (1971-11-01). "Some Epidemiological Clues in Thyroid Cancer". Archives of Internal Medicine. 128 (5): 755. doi:10.1001/archinte.1971.00310230085006. ISSN 0003-9926.
67. Raso, A. M.; Dorigo, M.; Terrando, R. (1975-11-30). "[Statistical analysis of correlations between tonsillectomy and malignant neoplasms of the thyroid]". Minerva Chirurgica. 30 (22): 1135–1139. ISSN 0026-4733. PMID 1228489.
68. H., Lubin, Jay; E., Burns, Patricia; J., Blot, William; W., Lees, Alan; Carol, May,; E., Morris, Linda; F., Fraumeni, Joseph (1982-02-01). "Risk Factors for Breast Cancer in Women in Northern Alberta, Canada, as Related to Age at Diagnosis". Journal of the National Cancer Institute. 68 (2). doi:10.1093/jnci/68.2.211. ISSN 0027-8874.
69. Brasky, Theodore M.; Bonner, Matthew R.; Dorn, Joan; Marhsall, James R.; Vena, John E.; Brasure, John R.; Freudenheim, Jo L. (2009-04-01). "Tonsillectomy and breast cancer risk in the Western New York Diet Study". Cancer Causes & Control. 20 (3): 369–374. doi:10.1007/s10552-008-9251-5. ISSN 0957-5243.
70. Sun, Li-Min; Chen, Hsuan-Ju; Li, Tsai-Chung; Sung, Fung-Chang; Kao, Chia-Hung (2015-01-01). "A nationwide population-based cohort study on tonsillectomy and subsequent cancer incidence". The Laryngoscope. 125 (1): 134–139. doi:10.1002/lary.24864. ISSN 1531-4995.
71. AS, Whittemore; Jr, Paffenbarger RS; K, Anderson; JE, Lee (1984-12-01). "Early precursors of urogenital cancers in former college men". The Journal of Urology. 132 (6): 1256–61. doi:10.1016/s0022-5347(17)50118-4. ISSN 0022-5347. PMID 6502830.
72. Zevallos, Jose P; Mazul, Angela L; Rodriguez, Nidia; Weissler, Mark C; Brennan, Paul; Anantharaman, Devasena; Abedi-Ardekani, Behnoush; Hayes, D Neil; Olshan, Andrew F (2016). "Previous tonsillectomy modifies odds of tonsil and base of tongue cancer". British Journal of Cancer. 114 (7): 832–838. doi:10.1038/bjc.2016.63. PMC 4984870 Freely accessible. PMID 26977858.
73. Paffenbarger, Ralph S.; Wing, Alvin L.; Hyde, Robert T. (1978-01-01). "Characteristics in Youth Predictive of Adult-Onset Malignant Lymphomas, Melanomas, and Leukemias: Brief Communications 2 3". Journal of the National Cancer Institute. 60 (1): 89–92. doi:10.1093/jnci/60.1.89. ISSN 0027-8874.
74. Schuz, J; Kaletsch, U; Meinert, R; Kaatsch, P; Michaelis, J (1999-05-01). "Association of childhood leukaemia with factors related to the immune system". British Journal of Cancer. 80 (3): 585–590. doi:10.1038/sj.bjc.6690395. ISSN 0007-0920. PMC 2362320 Freely accessible. PMID 10408870.
75. Cuneo, J. M. (1972-04-15). "Tonsillectomy and leukaemia". The Lancet. 1 (7755): 846–847. doi:10.1016/s0140-6736(72)90829-x. ISSN 0140-6736. PMID 4111604.
76. "Investigating pediatric cancer risk utilizing the Utah population database - ProQuest". search.proquest.com. Retrieved 2018-03-05.
77. Anderson, H. R.; Bland, J. M.; Peckham, C. S. (1987-06-01). "Risk factors for asthma up to 16 years of age. Evidence from a national cohort study". Chest. 91 (6 Suppl): 127S–130S. doi:10.1378/chest.91.6_supplement.127s. ISSN 0012-3692. PMID 3581954.
78. Byars, Sean G.; Stearns, Stephen C.; Boomsma, Jacobus J. (2018-06-07). "Association of Long-Term Risk of Respiratory, Allergic, and Infectious Diseases With Removal of Adenoids and Tonsils in Childhood". JAMA Otolaryngology–Head & Neck Surgery. doi:10.1001/jamaoto.2018.0614. ISSN 2168-6181.
79. Sultész, Monika; Katona, Gábor; Hirschberg, Andor; Gálffy, Gabriella (2010-05-01). "Prevalence and risk factors for allergic rhinitis in primary schoolchildren in Budapest". International Journal of Pediatric Otorhinolaryngology. 74 (5): 503–509. doi:10.1016/j.ijporl.2010.02.008.
80. Matheson, M. C.; Walters, E. H.; Simpson, J. A.; Wharton, C. L.; Ponsonby, A.-L.; Johns, D. P.; Jenkins, M. A.; Giles, G. G.; Hopper, J. L. (2009-03-01). "Relevance of the hygiene hypothesis to early vs. late onset allergic rhinitis". Clinical & Experimental Allergy. 39 (3): 370–378. doi:10.1111/j.1365-2222.2008.03175.x. ISSN 1365-2222.
81. Basseri, Robert J.; Chong, Kelly; Chang, Christopher; Pimentel, Mark (2011). "History of Tonsillectomy Is Associated With Irritable Bowel Syndrome". Journal of Clinical Gastroenterology:. 45 (10): 912. doi:10.1097/MCG.0b013e31822a289f.
82. Sun, Weili; Han, Xiao; Wu, Siyuan; Yang, Chuanhua (2016-06-01). "Tonsillectomy and the risk of inflammatory bowel disease: A systematic review and meta-analysis". Journal of Gastroenterology and Hepatology. 31 (6): 1085–1094. doi:10.1111/jgh.13273. ISSN 1440-1746.
83. Koutroubakis, I. E.; Vlachonikolis, I. G.; Kapsoritakis, A.; Spanoudakis, S.; Roussomoustakaki, M.; Mouzas, I. A.; Kouroumalis, E. A.; Manousos, O. N. (1999-02-01). "Appendectomy, tonsillectomy, and risk of inflammatory bowel disease". Diseases of the Colon & Rectum. 42 (2): 225–230. doi:10.1007/BF02237133. ISSN 0012-3706.
84. Gearry, Richard B; Richardson, Ann K; Frampton, Christopher M; Dodgshun, Andrew J; Barclay, Murray L (2010-02-01). "Population-based cases control study of inflammatory bowel disease risk factors". Journal of Gastroenterology and Hepatology. 25 (2): 325–333. doi:10.1111/j.1440-1746.2009.06140.x. ISSN 1440-1746.
85. Wurzelmann, John I.; Lyles, Cynthia M.; Sandler, Robert S. (1994-03-01). "Childhood infections and the risk of inflammatory bowel disease". Digestive Diseases and Sciences. 39 (3): 555–560. doi:10.1007/BF02088342. ISSN 0163-2116.
86. Spehlmann, Martina E.; Begun, Alexander Z.; Saroglou, Ekaterini; Hinrichs, Frank; Tiemann, Ute; Raedler, Andreas; Schreiber, Stefan (2012-02-01). "Risk factors in German twins with inflammatory bowel disease: Results of a questionnaire-based survey". Journal of Crohn's and Colitis. 6 (1): 29–42. doi:10.1016/j.crohns.2011.06.007. ISSN 1873-9946.
87. Ballester, J. C. Andreu; Ballester, F.; Rubio, E. Colomer; Scheiding, M. Millán (2005-03-01). "Association between tonsillectomy, adenoidectomy, and appendicitis". Revista Española de Enfermedades Digestivas. 97 (3). doi:10.4321/s1130-01082005000300006. ISSN 1130-0108.
88. Janszky, I.; Mukamal, K. J.; Dalman, C.; Hammar, N.; Ahnve, S. (2011-09-01). "Childhood appendectomy, tonsillectomy, and risk for premature acute myocardial infarction--a nationwide population-based cohort study". European Heart Journal. 32 (18): 2290–2296. doi:10.1093/eurheartj/ehr137. ISSN 0195-668X.
89. Sawahata, Michiru; Nakamura, Yosikazu; Sugiyama, Yukihiko (May 2017). "Appendectomy, tonsillectomy, and risk for sarcoidosis – A hospital-based case-control study in Japan". Respiratory Investigation. 55 (3): 196–202. doi:10.1016/j.resinv.2016.12.004.
90. F, Fernandez-Madrid; AH, Reed; RL, Karvonen; JL, Granda (1985-02-01). "Influence of antecedent lymphoid surgery on the odds of acquiring rheumatoid arthritis". The Journal of rheumatology. 12 (1): 43–8. ISSN 0315-162X. PMID 3981518.
91. NL, Gottlieb; WF, Page; DJ, Appelrouth; R, Palmer; IM, Kiem (1979). "Antecedent tonsillectomy and appendectomy in rheumatoid arthritis". The Journal of rheumatology. 6 (3): 316–23. ISSN 0315-162X. PMID 490526.
92. Duval, Melanie; Daniel, Sam J. (2008-12-01). "Retropharyngeal and parapharyngeal abscesses or phlegmons in children". International Journal of Pediatric Otorhinolaryngology. 72 (12): 1765–1769. doi:10.1016/j.ijporl.2008.07.007. ISSN 0165-5876.
93 Marchisio, P.; Principi, N.; Passali, D.; Salpietro, D. C.; Boschi, G.; Chetrì, G.; Caramia, G.; Longhi, R.; Reali, E. (July 1998). "Epidemiology and treatment of otitis media with effusion in children in the first year of primary school". Acta Oto-Laryngologica. 118 (4): 557–562. doi:10.1080/00016489850154720. ISSN 0001-6489. PMID 9726683.
94. Poskanzer, DavidC. (1965-12-18). "TONSILLECTOMY AND MULTIPLE SCLEROSIS". The Lancet. Originally published as Volume 2, Issue 7425. 286 (7425): 1264–1266. doi:10.1016/S0140-6736(65)92281-6.
95. Lamoureux, G.; Giard, N.; Jolicoeur, R.; Toughlian, V.; Desrosiers, M. (1976-01-24). "Immunological features in multiple sclerosis". The BMJ. 1 (6003): 183–186. doi:10.1136/bmj.1.6003.183. ISSN 0007-1447. PMC 1638425 Freely accessible. PMID 764920.
96. Grønning, Marit; Riise, Trond; Kvåle, Gunnar; Albrektsen, Grethe; Midgard, Rune; Nyland, Harald (1993). "Infections in Childhood and Adolescence in Multiple Sclerosis". Neuroepidemiology. 12 (2): 61–69. doi:10.1159/000110302.
97. Lunny, Carole; Knopp-Sihota, Jennifer A.; Fraser, Shawn N. (2013-01-01). "Surgery and risk for multiple sclerosis: a systematic review and meta-analysis of case–control studies". BMC Neurology. 13: 41. doi:10.1186/1471-2377-13-41. ISSN 1471-2377. PMC 3651719 Freely accessible. PMID 23648120.
98. Wang, Ying-Piao; Wang, Mao-Che; Lin, Hung-Ching; Lee, Kuo-Sheng; Chou, Pesus (2015-04-07). "Tonsillectomy and the Risk for Deep Neck Infection—A Nationwide Cohort Study". PLOS One. 10 (4): e0117535. doi:10.1371/journal.pone.0117535. ISSN 1932-6203. PMC 4388732 Freely accessible. PMID 25849535.
99. Ogra, Pearay L. (2010-01-14). "Effect of Tonsillectomy and Adenoidectomy on Nasopharyngeal Antibody Response to Poliovirus". dx.doi.org/10.1056/NEJM197101142840201. doi:10.1056/nejm197101142840201. Retrieved 2017-03-15.
100. Francis, Thomas; Krill, Carl E.; Toomey, John A.; Mack, Walter N. (1942-08-22). "POLIOMYELITIS FOLLOWING TONSILLECTOMY IN FIVE MEMBERS OF A FAMILY: AN EPIDEMIOLOGIC STUDY". JAMA: The Journal of the American Medical Association. 119 (17): 1392–1396. doi:10.1001/jama.1942.02830340004002. ISSN 0002-9955.
101. Anderson, John A. (1945). "Poliomyelitis and recent tonsillectomy". The Journal of Pediatrics. 27 (1): 68–70. doi:10.1016/s0022-3476(45)80208-1.
102. Barsky, Percy; Lauer, Ronald (1957-09-15). "Tonsillectomy and the Risk of Poliomyelitis". Canadian Medical Association Journal. 77 (6): 576–578. ISSN 0008-4409. PMC 1824413 Freely accessible. PMID 13460884.
103. Karppelin, M.; Siljander, T.; Huhtala, H.; Aromaa, A.; Vuopio, J.; Hannula-Jouppi, K.; Kere, J.; Syrjänen, J. (2012-09-25). "Recurrent cellulitis with benzathine penicillin prophylaxis is associated with diabetes and psoriasis". European Journal of Clinical Microbiology & Infectious Diseases. 32 (3): 369–372. doi:10.1007/s10096-012-1751-2. ISSN 0934-9723.
104. Parikh-Patel, Arti; Gold, Ellen B.; Worman, Howard; Krivy, Kathryn E.; Gershwin, M. Eric (2001-01-01). "Risk factors for primary biliary cirrhosis in a cohort of patients from the United States". Hepatology. 33 (1): 16–21. doi:10.1053/jhep.2001.21165. ISSN 1527-3350.
105. Gershwin, M. Eric; Selmi, Carlo; Worman, Howard J.; Gold, Ellen B.; Watnik, Mitchell; Utts, Jessica; Lindor, Keith D.; Kaplan, Marshall M.; Vierling, John M. (2005-11-01). "Risk factors and comorbidities in primary biliary cirrhosis: A controlled interview-based study of 1032 patients". Hepatology. 42 (5): 1194–1202. doi:10.1002/hep.20907. ISSN 1527-3350. PMC 3150736 Freely accessible. PMID 16250040.
106. Chung, Shiu-Dong; Lin, Herng-Ching; Wu, Chuan-Song; Kao, Li-Ting; Hung, Shih-Han (December 2016). "A tonsillectomy increased the risk of chronic rhinosinusitis among children: A three-year follow-up study". International Journal of Pediatric Otorhinolaryngology. 91: 82–85. doi:10.1016/j.ijporl.2016.09.038.
107. Murphy, Tanya K.; Storch, Eric A.; Lewin, Adam B.; Edge, Paula J.; Goodman, Wayne K. (2012-02-01). "Clinical Factors Associated with Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections". The Journal of Pediatrics. 160 (2): 314–319. doi:10.1016/j.jpeds.2011.07.012. ISSN 0022-3476. PMC 3227761 Freely accessible. PMID 21868033.
108. A, Cantani; P, Bellioni; F, Salvinelli; L, Businco (1986-12-01). "Serum immunoglobulins and secretory IgA deficiency in tonsillectomized children". Annals of Allergy. 57 (6): 413–6. ISSN 0003-4738. PMID 3789468.
109. Andreu-Ballester, Juan Carlos; Pérez-Griera, Jaime; Ballester, Ferran; Colomer-Rubio, Enrique; Ortiz-Tarín, Inmaculada; Peñarroja Otero, Carlos (2007-06-01). "Secretory immunoglobulin A (sIgA) deficiency inserum of patients with GALTectomy (appendectomy and tonsillectomy)". Clinical Immunology. 123 (3): 289–297. doi:10.1016/j.clim.2007.02.004.
110. P, Brandtzaeg (1996-01-01). "The B-cell development in tonsillar lymphoid follicles". Acta Oto-Laryngologica Supplementum. 523: 55–9. ISSN 0365-5237. PMID 9082810.
111. Kim, Jonathan; Morris, Michael. "Long-Term Effects of Tonsillectomy on Immunity" (PDF). Georgetown University School of Medicine, Washington, D.C.
112. Ji, Jianguang; Sundquist, Jan; Sundquist, Kristina (2016-08-01). "Tonsillectomy associated with an increased risk of autoimmune diseases: A national cohort study". Journal of Autoimmunity. 72: 1–7. doi:10.1016/j.jaut.2016.06.007.
113. Mészáros, D.; Dharmage, S. C.; Matheson, M. C.; Venn, A.; Wharton, C. L.; Johns, D. P.; Abramson, M. J.; Giles, G. G.; Hopper, J. L. (2010-06-01). "Poor lung function and tonsillectomy in childhood are associated with mortality from age 18 to 44". Respiratory Medicine. 104 (6): 808–815. doi:10.1016/j.rmed.2009.12.001. ISSN 0954-6111. PMID 20079616.
114. Johansson, Ewa; Hultcrantz, Elisabeth (2003-09-01). "Tonsillectomy—clinical consequences twenty years after surgery?". International Journal of Pediatric Otorhinolaryngology. 67 (9): 981–988. doi:10.1016/S0165-5876(03)00196-4. ISSN 0165-5876. PMID 12907054.
|