
手臂上的疤痕组织
疤痕是纤维组织的一个区域,在受伤后取代正常皮肤。疤痕来自皮肤以及身体其他器官和组织中伤口修复的生物学过程。因此,瘢痕形成是愈合过程的自然部分。除了非常轻微的病变之外,每个伤口(例如,在事故,疾病或手术后)都会导致一定程度的瘢痕形成。一个例外是具有完全再生的动物,其再生组织而没有瘢痕形成。
瘢痕组织由与其取代的组织相同的蛋白质(胶原蛋白)组成,但蛋白质的纤维组成不同;而不是在正常组织中发现的胶原纤维的随机篮网形成,在纤维化中,胶原交联并在单一方向上形成明显的排列。[1]这种胶原瘢痕组织排列通常具有比正常胶原随机排列更差的功能质量。例如,皮肤上的疤痕对紫外线辐射的抵抗力较弱,汗腺和毛囊不会在疤痕组织内生长。[2]心肌梗塞,通常称为心脏病发作,导致心肌中的瘢痕形成,这导致肌肉力量的丧失和可能的心力衰竭。然而,有一些组织(例如骨骼)可以愈合而没有任何结构或功能恶化。
目录
1 类型
1.1 肥厚
1.2 瘢痕疙瘩
1.3 萎缩
1.4 妊娠纹
1.5 脐
2 病理生理学
2.1 胶原蛋白合成
3 治疗
3.1 化学换肤
3.2 填料注射
3.3 激光治疗
3.4 放疗
3.5 修整
3.6 类固醇
3.7 手术
3.8 维生素
3.9 其他
4 社会与文化
4.1 故意留下疤痕
4.2 词源
5 研究
6 参考
类型

有可见面部伤痕的人。
所有疤痕都由与其替代的组织相同的胶原组成,但与正常组织相比,瘢痕组织的组成是不同的。[1]与分散纤维弹性的正常组织不同,瘢痕组织也缺乏弹性[3]。疤痕在过量表达的胶原蛋白量方面不同。标签已应用于过度表达的差异。两种最常见的类型是肥厚性和瘢痕疙瘩,[4]两者都经历过度僵硬的胶原蛋白束生长过度扩张组织,阻止组织再生。另一种形式是萎缩性瘢痕形成(凹陷性瘢痕形成),其还具有过度抑制胶原蛋白阻断再生的作用。这种疤痕类型是凹陷的,因为胶原蛋白束不会过度扩张组织。拉伸痕迹(striae)被一些人认为是伤疤。
高黑色素水平以及非洲或亚洲血统可能使不良瘢痕更加明显。[5]
肥厚
当身体过度生成胶原蛋白时会发生肥厚性疤痕,导致疤痕在周围皮肤上方升高。肥厚性瘢痕呈现皮肤上红色凸起的肿块。它们通常在伤口感染或伤口闭合后4至8周内发生,伴有过度紧张和/或其他创伤性皮肤损伤。[4]
瘢痕疙瘩
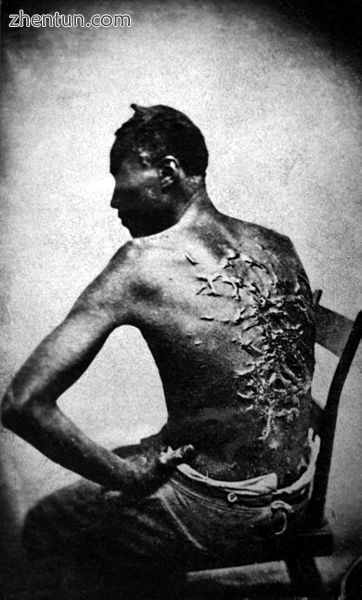
继续鞭打后瘢痕疙瘩。皮肤色素沉着较深的人更容易发生瘢痕疙瘩。
瘢痕疙瘩是一种更严重的过度瘢痕形成,因为它们可以无限长地生长成大的肿瘤(虽然是良性)肿瘤。[4]
肥厚性瘢痕通常与瘢痕疙瘩的区别在于它们在原始伤口区域之外缺乏生长,但这种常见的区别可能导致混淆。[6]
瘢痕疙瘩可能发生在任何人身上,但在黑皮肤的人中最常见。[7]它们可能由手术,意外,痤疮或有时身体穿孔引起。在一些人中,瘢痕疙瘩自发形成。虽然它们可能是一个美容问题,但瘢痕疙瘩只是胶原蛋白的惰性团块,因此完全无害,不会发生癌变。然而,在某些人身上,它们可能会发痒或疼痛。它们往往在肩膀和胸部最常见。肥厚性瘢痕和瘢痕疙瘩在次要意图闭合的伤口中更常见[8]。手术切除瘢痕疙瘩是有风险的,可能会使瘢痕疙瘩的病情恶化。
萎缩性
萎缩性瘢痕呈现皮肤凹陷凹陷的形式,具有凹陷外观。这些是在支撑皮肤的基础结构(例如脂肪或肌肉)丢失时引起的。这种类型的疤痕通常与痤疮,[9] [10]水痘,其他疾病(特别是葡萄球菌感染),手术,某些昆虫和蜘蛛叮咬或事故有关。它也可能由遗传性结缔组织疾病引起,如Ehlers-Danlos综合征[11]。
妊娠纹
主要文章:妊娠纹
妊娠纹(技术上称为皮纹)也是一种疤痕形成。 这些是在皮肤快速拉伸时引起的(例如在怀孕期间[12] 显着的体重增加,或青春期生长突增),[13]或在愈合过程中皮肤处于紧张状态时(通常在关节)。 这种类型的疤痕通常会在几年后改善外观。[12]
皮质类固醇水平升高与皮纹发育有关[14]。
脐
人类和其他胎盘哺乳动物的脐带疤痕(通常称为肚脐)在出生后切断脐带时开始愈合。 产卵动物有脐带疤痕,根据物种的不同,可能在生命中保持可见或在出生后几天内消失。[15] [16]
病理生理学

右侧道皮疹一年后出现肥厚性瘢痕,左侧原始伤口。
疤痕是组织损伤后身体修复机制的产物。如果伤口在两周内迅速愈合,新形成的皮肤,将会沉积最少的胶原蛋白,并且不会形成疤痕。[17]当细胞外基质感知到机械应力负荷增加时,组织会出现疤痕,[18]并且疤痕会受到应力遮挡伤口的限制。[18] 2mm以下的小全厚度伤口快速恢复并且无疤痕愈合。[19] [20]深度二度烧伤愈合,伴有疤痕和脱发。[2]疤痕组织中不会形成汗腺,这会损害体温的调节。[21]在3个月以下的瘢痕组织中通常不会检测到弹性纤维。[22]在疤痕中,网钉丢失; [23]通过缺乏网钉疤痕往往比正常组织更容易剪切。[23]
子宫内膜是子宫的内层,是唯一可以快速循环脱落和再生而不留疤痕的成人组织;每月在7天的窗口内大致减少和恢复。[24]所有其他成人组织在快速脱落或受伤后都会出现疤痕。
可能发生长时间炎症以及成纤维细胞增殖[25]。经常在皮肤受伤后发红不是疤痕,通常不是永久性的(见伤口愈合)。然而,这种红色消散所需的时间可能是几天到几年之内,在一些严重和罕见的情况下,需要几年。
根据身体受伤的位置和受伤者的年龄,疤痕形成不同。
初始损伤越严重,疤痕通常就越严重。
当真皮(深层,厚厚的皮肤层)受损时会出现皮肤疤痕。大多数皮肤疤痕是扁平的,并留下造成它们的原始伤害的痕迹。
允许继发愈合的伤口往往比初次闭合伤口更容易疤痕。[8]
胶原蛋白合成
在伤口完全愈合之前,任何伤害都不会成为伤疤;在最严重的病理情况下,例如瘢痕疙瘩可能需要数月或数年。为了开始修补损伤,会产生凝块;凝块是导致临时矩阵的开始过程。在该过程中,第一层是临时基质并且不是疤痕。随着时间的推移,受伤的身体组织然后在临时基质内过度表达胶原蛋白以产生胶原基质。这种胶原蛋白过度表达持续并使胶原基质内的纤维排列交联,使胶原蛋白致密。这种密集的胶原蛋白,变成无弹性的白色胶原蛋白[25]疤痕壁,阻止细胞通讯和再生;结果,产生的新组织将具有与周围未受伤组织不同的纹理和质量。这种延长的胶原蛋白生成过程导致了富有的疤痕。
成纤维细胞
瘢痕形成是由成纤维细胞增殖引起的,[25]这一过程始于对凝块的反应。[26]
为了修复损伤,成纤维细胞慢慢形成胶原瘢痕。成纤维细胞增殖是圆形的[27]并且周期性地,成纤维细胞增殖在临时和胶原基质内铺设厚而白色的胶原[25],导致纤维上丰富的胶原蛋白产生[25] [26] [28]给它们不均匀的疤痕纹理。随着时间的推移,成纤维细胞继续在基质周围爬行,调整更多的纤维,并且在此过程中,疤痕沉淀并变硬。[29]这种成纤维细胞增殖也使组织收缩。[27] [30]在未受伤的组织中,这些纤维不会被厚胶原蛋白过度表达而不会收缩。
肌成纤维细胞
参与瘢痕形成和收缩的成纤维细胞是肌成纤维细胞[31],它是一种特殊的收缩性成纤维细胞。[32]这些细胞表达α-平滑肌肌动蛋白(α-SMA)。[33]
肌成纤维细胞在胚胎阶段的第一个三个月中不存在,其中损伤愈合无瘢痕; [19]小切口或切除伤口小于2毫米,也可愈合而无瘢痕; [19]在成人未受伤的组织中成纤维细胞本身被捕;然而,肌成纤维细胞在成人伤口愈合中大量发现,可以治愈疤痕。[32]
肌原纤维细胞构成在愈合开始时在胚后伤口中增殖的高比例的成纤维细胞。例如,在大鼠模型中,肌成纤维细胞可构成高达70%的成纤维细胞,[31]并且是造成组织纤维化的原因[34]。一般来说,肌成纤维细胞在30天内从伤口消失[35],但可以在肥大的病理情况下保持,例如瘢痕疙瘩。[32] [35]肌成纤维细胞具有可塑性,并且通过毛囊的再生可以将小鼠转化为脂肪细胞而不是瘢痕组织。[36] [37]
治疗
早期有效治疗痤疮疤痕可以预防严重的痤疮和经常发生的疤痕。[38]截至2014年,没有用于治疗或预防疤痕的处方药。[39]
化学换肤
化学换肤是一种化学物质,可以控制的方式破坏表皮,导致去角质和减轻某些皮肤状况,包括浅表性痤疮疤痕。[40]根据果皮的深度,可以使用各种化学品,应谨慎使用,特别是对于深色皮肤的个体和易患瘢痕疙瘩或有活动性感染的个体。[41]
填料注射
填充胶原蛋白可用于将萎缩性疤痕提升至周围皮肤的水平。[42]风险因使用的填充物而异,可能包括进一步的毁容和过敏反应。[43]
激光治疗
非烧蚀激光,如585 nm脉冲染料激光,1064 nm和1320 nm Nd:YAG,或1540 nm Er:玻璃,可用作增生性瘢痕和瘢痕疙瘩的激光治疗。[44]对于烧伤疤痕,它们可以改善外观。[45]
诸如二氧化碳激光(CO2)或Er:YAG之类的烧蚀激光为萎缩性和痤疮疤痕提供了最佳效果。[46]像皮肤磨削一样,烧蚀激光通过将表皮破坏到一定深度来起作用。与非消融治疗相比,消融治疗的愈合时间更长,风险更高;然而,非消融疗法仅对萎缩性和痤疮疤痕的美容外观提供微小的改善。[44]
放射治疗
低剂量,浅表放疗有时用于预防严重瘢痕疙瘩和肥厚性瘢痕的复发。尽管缺乏临床试验,但它被认为是有效的,但由于存在长期副作用的风险,因此仅用于极端情况。[47]
敷料
有机硅疤痕治疗通常用于预防疤痕形成和改善现有的疤痕外观。[48] Cochrane合作的一项元素研究发现,有缺陷的证据表明有机硅凝胶薄膜有助于防止疤痕形成。[49]然而,检查它的研究质量很差,容易产生偏见。[49]
压力敷料通常用于治疗烧伤和肥厚性疤痕,但缺乏支持证据。[50]然而,护理提供者通常报告改善,并且压力治疗在治疗耳部瘢痕疙瘩方面是有效的。[50]一般认为治疗有效可能会阻止其在临床试验中进一步研究。[50]
类固醇
皮质类固醇注射到瘢痕中的长期疗程可能有助于压平和软化瘢痕疙瘩或肥厚性瘢痕的外观。[51]
外用类固醇无效。[52]然而,丙酸氯倍他索可用作瘢痕疙瘩的替代疗法。[53]
手术

痤疮引起的疤痕(左)和疤痕翻修手术后一天的照片:缝合线周围的区域仍然因手术而肿胀。
疤痕修复是切除疤痕组织的过程。切除后,新伤口通常通过主要意图闭合至愈合,而非次要意图。更深的切割需要多层闭合才能最佳地愈合,否则会导致下陷或凹陷的疤痕。[54]
手术切除肥厚性或瘢痕性瘢痕通常与其他方法相关,例如压迫疗法或硅凝胶片。然而,单独切除瘢痕疙瘩显示复发率接近45%。目前正在进行一项临床研究,以评估手术和激光辅助治疗在肥厚性或瘢痕疙瘩中的治疗效果。
决定是用于治疗痤疮或其他皮肤病留下的深滚疤痕的过程。它也用于减轻严重的眉间线的出现,尽管它在这种应用中的有效性值得商榷。基本上该过程涉及将受影响区域中的皮肤组织与较深的瘢痕组织分离。这允许血液在受影响的区域下汇集,最终导致深滚疤痕与皮肤区域的其余部分平齐。一旦皮肤变平,可以使用激光换肤,微晶换肤术或化学换肤等治疗来消除疤痕组织。
维生素
研究表明,使用维生素E和洋葱提取物(以Mederma出售)作为治疗疤痕是无效的。[50]维生素E在高达33%的使用者中引起接触性皮炎,在某些情况下,它可能会使疤痕外观恶化,并可能引起轻微的皮肤刺激[52],但维生素C及其一些酯类会褪色与某些疤痕相关的暗色素。[55] ]
其他
化妆品;医疗化妆可以暂时掩盖伤疤。[56]这最常用于面部疤痕。
皮肤磨削术涉及使用特殊设备去除皮肤表面,并且通常涉及局部麻醉。
按摩在瘢痕治疗方面的效果很弱。手术切口产生的伤口比创伤性伤口或烧伤伤口的任何有益效果更大。[57]
微针 [58]
社会与文化
故意伤痕累累
主要文章:划痕
疤痕的持久性导致其在一些文化和亚文化中被故意用作人体艺术的一种形式。世界各地的许多团体和文化都可以找到这些形式的仪式和非仪式疤痕练习。
词源
在14世纪后期首次用英语证实,疤痕这个词源于古法语escharre的混合,来自晚期拉丁语eschara,[59]这是希腊语ἐσχάρα(eskhara)的拉丁化,意思是“壁炉”,但在药物中“结痂,焦灼伤引起的烧伤或其他,[60] [61]和中古英语skar(”切割,裂缝,切口“),来自OldNorseskare(”缺口,间隙“)。[这种混合有助于形成英语的意义。比较斯卡伯勒的skare演变为疤痕。
研究
正在测试皮内注射转化生长因子β3(TGFβ3)。已经完成的三项试验的结果发表在“柳叶刀”上,并附有一篇社论评论。[63]
一项研究表明蛋白质核糖体s6激酶(RSK)在瘢痕组织的形成中发现,引入一种抵抗RSK的化学物质可以阻止肝硬化的形成。这种治疗还有可能减少甚至完全阻止其他类型的瘢痕形成。[64]
研究还表明骨桥蛋白可能与瘢痕形成有关[65] [66]。
参考:
Sherratt, Jonathan A. (2010). "Mathematical Modelling of Scar Tissue Formation". Department of Mathematics, Heriot-Watt University. Retrieved 20 August 2010. This is composed of the same main protein (collagen) as normal skin, but with differences in details of composition. Most crucially, the protein fibres in normal tissue have a random (basketweave) appearance, while those in scar tissue have pronounced alignment in a single direction.
John Kraft; Charles Lynde, MD, FRCPC. "Giving Burns the First, Second and Third Degree - Classification of burns". skincareguide.ca. Retrieved 31 January 2012. Formation of a thick eschar, slow healing (>1month), Obvious scarring, hair loss.
A. Bernard Ackerman, MD, Almut Böer, MD, Bruce Bennin, MD, Geoffrey J. Gottlieb, MD (January 2005). Histologic Diagnosis of Inflammatory Skin Diseases An Algorithmic Method Based on Pattern Analysis: Embryologic, Histologic, and Anatomic Aspects: Elastic Fibers (Third ed.). Ardor Scribendi. p. 522. ISBN 9781893357259.
Gauglitz GG, Korting HC, Pavicic T, Ruzicka T, Jeschke MG (January–February 2011). "Hypertrophic Scarring and Keloids: Pathomechanisms and Current and Emerging Treatment Strategies". Mol Med. 17 (1–2): 113–125. doi:10.2119/molmed.2009.00153. PMC 3022978. PMID 20927486.
Kelly AP (2009). "Update on the Management of Keloids". Seminars in Cutaneous Medicine and Surgery. 28 (2): 71–76. doi:10.1016/j.sder.2009.04.002. PMID 19608056.
Roseborough IE, Grevious MA, Lee RC (January 2004). "Prevention and treatment of excessive dermal scarring". J Natl Med Assoc. 96 (1): 108–16. PMC 2594768. PMID 14746360.
Martini, Frederic H. (2006). Fundamentals of Anatomy & Physiology, Seventh Edition, p. 171. Benjamin Cummings, San Francisco.
"Practical Plastic Surgery for Nonsurgeons - Secondary Wound Closure - Scarring" (PDF). Archived from the original (PDF) on 2016-08-26. Retrieved 2017-01-11. Wounds that are allowed to heal secondarily tend to have larger and more noticeable scars than the scars that results from primary closure. Secondary healing also has a greater tendency for hypertrophic scar/keloid formation. (page 86)
Goodman GJ (2000). "Postacne scarring: A review of its pathophysiology and treatment". Dermatologic Surgery. 26 (9): 857–871. doi:10.1046/j.1524-4725.2000.99232.x. PMID 10971560.
Fabbrocini G, Annunziata MC, D'Arco V, De Vita V, Lodi G, Mauriello MC, Pastore F, Monfrecola G (2010). "Acne Scars: Pathogenesis, Classification and Treatment". Dermatology Research and Practice. 2010: 1–13. doi:10.1155/2010/893080. PMC 2958495. PMID 20981308.
"Clinical manifestations and diagnosis of Ehlers-Danlos syndromes". www.uptodate.com. Retrieved 2017-06-15.
Young, G.; Jewell, D. (1996). "Creams for preventing stretch marks in pregnancy". In Young, Gavin. Cochrane Database of Systematic Reviews. The Cochrane Database of Systematic Reviews. pp. CD000066. doi:10.1002/14651858.CD000066. PMID 10796111.
Elsaie ML, Baumann LS, Elsaaiee LT (2009). "Striae Distensae (Stretch Marks) and Different Modalities of Therapy: An Update". Dermatologic Surgery. 35 (4): 563–573. doi:10.1111/j.1524-4725.2009.01094.x. PMID 19400881.
Hengge UR, Ruzicka T, Schwartz RA, Cork MJ (2006). "Adverse effects of topical glucocorticosteroids". Journal of the American Academy of Dermatology. 54 (1): 1–15. doi:10.1016/j.jaad.2005.01.010. PMID 16384751.
"What Types of Animals Have Been to Space and More Questions From our Readers", Smithsonian Magazine May 2012, https://www.smithsonianmag.com/a ... r-readers-63029589/ Retrieved 25 November 2017
Flat-tailed horned lizard (Phrynosoma mcallii), US Fish & Wildlife Service https://www.fws.gov/southwest/es ... d%20Lizard%20RB.pdf Retrieved 25 November 2017
"POST BURN SCAR RELATIVE TO RE-EPITHELIALIZATION" (PDF). eplasty.com. 2011. Retrieved 6 February 2016. Healing in 2 weeks – minimal to no scar; Healing in 3 weeks – minimal to no scar except in high risk scar formers;Healing in 4 weeks or more – hypertrophic in more than 50% of patients
Victor W.Wong, SatoshiAkaishi, Michael T.Longaker, Geoffrey C.Gurtner (2011). "Pushing Back: Wound Mechanotransduction in Repair and Regeneration". sciencedirect.com. Journal of Investigative Dermatology. Retrieved 17 October 2018.
Traci A. Wilgus (9 March 2008). "Regenerative Healing in Fetal Skin: A Review of the Literature". o-wm.com. Retrieved 26 March 2011. Studies in sheep have indicated that myofibroblasts are absent in early scarless fetal wounds but are present during healing at later stages when prominent scarring occurs. In addition, incisional or small excisional wounds (2 mm) heal without a scar and do not contain myofibroblasts. In contrast, larger excisional wounds that heal with a scar contain strong a-SMA staining, with the number of myofibroblasts correlating with the size of the wound and amount of scarring.
Tam, Joshua; Wang, Ying; Vuong, Linh N.; Fisher, Jeremy M.; Farinelli, William A.; Anderson, R. Rox (2016). "Reconstitution of full-thickness skin by microcolumn grafting". Journal of Tissue Engineering and Regenerative Medicine. 11 (10): 2796–2805. doi:10.1002/term.2174. PMC 5697650. PMID 27296503.
Fu XB, Sun TZ, Li XK, Sheng ZY (February 2005). "Morphological and distribution characteristics of sweat glands in hypertrophic scar and their possible effects on sweat gland regeneration". Chinese Medical Journal. 118 (3): 186–91. PMID 15740645. Archived from the original on 2018-06-20. In hypertrophic scar tissue, no sweet gland and hair follicle exist usually because of the dermal and epidermal damage in extensive thermal skin injury, thus impairing regulation of body temperature
Roten SV1, Bhat S, Bhawan J. (February 1996). "Elastic fibers in scar tissue". J Cutan Pathol. 23 (1): 37–42. doi:10.1111/j.1600-0560.1996.tb00775.x. PMID 8720985.
Ira D. Papel (2011). Facial Plastic and Reconstructive Surgery (Third ed.). USA: Thieme Medical Publishers. p. 7. ISBN 9781588905154.
"Endometrial repair". princehenrys.org. 18 September 2012. Archived from the original on 2009-09-14. Retrieved 30 June 2013. Importantly, the endometrium is the only adult tissue to undergo rapid cyclic repair without scarring.
"Facts about fibroblast: scar tissue formation". Britannica.com. Retrieved 19 April 2010. As part of the healing process, specialized cells called fibroblasts in adjacent areas of skin produce a fibrous connective tissue made up of collagen. The bundles formed by these whitish, rather inelastic fibres make up the bulk of the scar tissue...
Parlange, Mary (17 December 2007). "New mechanical insights into wound healing and scar tissue formation". école Polytechnique Fédérale de Lausanne. eurekalert.org. Retrieved 28 August 2010. The body launches a complex rescue operation. Specialized cells called fibroblasts lurking just beneath the surface of the skin jump into action, enter the provisional wound matrix (the clot) and start secreting collagen to close the wound as fast as possible.
Parlange, Mary (17 December 2007). "New mechanical insights into wound healing and scar tissue formation". école Polytechnique Fédérale de Lausanne. eurekalert.org. Retrieved 28 August 2010. In the process, it liberates yet more growth factor that in turn stimulates other fibroblasts to become contractile…
Chen J, Jia-Han W, Hong-Xing Z (September 2005). "Inhibitory effects of local pretreated epidermis on wound scarring: a feasible method to minimize surgical scars". Burns. 31 (6): 758–64. doi:10.1016/j.burns.2005.04.002. PMID 16006045.
Wipff PJ, Rifkin DB, Meister JJ, Hinz B (December 2007). "Myofibroblast contraction activates latent TGF-beta1 from the extracellular matrix". The Journal of Cell Biology. 179 (6): 1311–23. doi:10.1083/jcb.200704042. PMC 2140013. PMID 18086923. Lay summary – école Polytechnique Fédérale de Lausanne (December 17, 2007).
Parlange, Mary (17 December 2007). "New mechanical insights into wound healing and scar tissue formation". école Polytechnique Fédérale de Lausanne. eurekalert.org. Retrieved 28 August 2010. The matrix grows stiffer and, at a certain point, the fibroblasts stop migrating and, like Popeye, change into powerful contractile cells, anchoring themselves to the matrix and pulling the edges of the wound together.
Linge, Claire (Harrow, GB), Mackie, Ian Paul (Sheffield, GB). "Method of preventing or reducing scarring of human skin". freepatentsonline.com. Retrieved 26 March 2010. myofibroblasts become differentiated from other cells in the wound within a few days after the onset of healing, and in the rat model can reach a peak where about 70% of the fibroblastic cells present are of the myofibroblast phenotype.
Linge, Claire (Harrow, GB), Mackie, Ian Paul (Sheffield, GB). "Method of preventing or reducing scarring of human skin". freepatentsonline.com. Retrieved 26 March 2010. These cells, which differentiate from the unwounded tissue cell type (fibroblasts), are responsible for laying down scar tissue. Indeed myofibroblasts remain present in hypertrophic scars up to four years after the original wounding event. An in vitro assay was accordingly developed to identify actives which prevent or reduce myofibroblast formation and thus identify actives which are effective in reducing and/or preventing scar tissue formation.
Traci A. Wilgus (9 March 2008). "Regenerative Healing in Fetal Skin: A Review of the Literature". o-wm.com. Retrieved 26 March 2011. Aside from normal fibroblasts, myofibroblasts, specialized contractile fibroblasts, also can contribute to wound repair. These cells express a-smooth muscle actin (a-SMA) and are characterized using transmission electron microscopy by a well-developed rough endoplasmic reticulum, nuclei with irregular borders, secretory vesicles denoting active collagen synthesis, and organized microfilament bundles.
Leask, Andrew (23 September 2008). "When Healing Turns To Scarring: Research Reveals Why It Happens And How To Stop It". the Canadian Foundation for Innovation, CIHR, the Arthritis Research Campaign, the Reynaud's and Scleroderma Foundation, and the Scleroderma Society.: sciencedaily.com. Retrieved 26 February 2011. During tissue repair, specialized cells called myofibroblasts migrate to the wound where they generate the adhesive and tensile forces required for wound closure. Normally, these myofibroblasts then disappear from the wound. But if they persist and continue to make connective tissue, it can become too thick, preventing the organ from functioning properly.
Linge, Claire (Harrow, GB), Mackie, Ian Paul (Sheffield, GB). "Method of preventing or reducing scarring of human skin". freepatentsonline.com. Retrieved 26 March 2010. the number of myofibroblasts present in the forming scar tissue begins to reduce via apoptosis, until by about 30 days no myofibroblasts are obvious within the scar.
Plikus; et al. (5 January 2017). "Regeneration of fat cells from myofibroblasts during wound healing". Science. 355 (6326): 748–752. doi:10.1126/science.aai8792. PMC 5464786. PMID 28059714.
Horsley, Watt (6 April 2017). "Repeal and Replace: Adipocyte Regeneration in Wound Repair". Cell Stem Cell (Submitted manuscript). 20 (4): 424–426. doi:10.1016/j.stem.2017.03.015. PMID 28388424.
"What is a Scar". American Academy of Dermatology. 2011. Retrieved 25 August 2011. Early and effective acne treatment can prevent severe acne and the scarring that often follows
Ferguson MW, O'Kane S (May 2004). "Scar-free healing: from embryonic mechanisms to adult therapeutic intervention". Philos. Trans. R. Soc. Lond. B Biol. Sci. 359 (1445): 839–50. doi:10.1098/rstb.2004.1475. PMC 1693363. PMID 15293811.
Khunger N (January 2008). "Standard guidelines of care for acne surgery". Indian Journal of Dermatology, Venereology and Leprology. 74 Suppl: S28–36. PMID 18688101.
Khunger N (January 2008). "Standard guidelines of care for chemical peels". Indian Journal of Dermatology, Venereology and Leprology. 74 Suppl: S5–12. PMID 18688104.
Cooper JS, Lee BT (December 2009). "Treatment of facial scarring: lasers, filler, and nonoperative techniques". Facial Plastic Surgery. 25 (5): 311–5. doi:10.1055/s-0029-1243079. PMID 20024872.
Lemperle G, Rullan PP, Gauthier-Hazan N (September 2006). "Avoiding and treating dermal filler complications". Plastic and Reconstructive Surgery. 118 (3 Suppl): 92S–107S. doi:10.1097/01.prs.0000234672.69287.77. PMID 16936549.
Elsaie ML, Choudhary S (November 2010). "Lasers for scars: a review and evidence-based appraisal". Journal of Drugs in Dermatology. 9 (11): 1355–62. PMID 21061757.
Willows, BM; Ilyas, M; Sharma, A (4 August 2017). "Laser in the management of burn scars". Burns. 43 (7): 1379–1389. doi:10.1016/j.burns.2017.07.001. PMID 28784339.
Khatri KA, Mahoney DL, McCartney MJ (April 2011). "Laser scar revision: A review". Journal of Cosmetic and Laser Therapy. 13 (2): 54–62. doi:10.3109/14764172.2011.564625. PMID 21401378.
Ogawa R, Yoshitatsu S, Yoshida K, Miyashita T (October 2009). "Is radiation therapy for keloids acceptable? The risk of radiation-induced carcinogenesis". Plastic and Reconstructive Surgery. 124 (4): 1196–201. doi:10.1097/PRS.0b013e3181b5a3ae. PMID 19935303.
Stavrou D, Weissman O, Winkler E, Yankelson L, Millet E, Mushin OP, Liran A, Haik J (October 2010). "Silicone-based scar therapy: a review of the literature". Aesthetic Plastic Surgery. 34 (5): 646–51. doi:10.1007/s00266-010-9496-8. PMID 20354695.
O'Brien, L; Jones, DJ (12 September 2013). "Silicone gel sheeting for preventing and treating hypertrophic and keloid scars". The Cochrane Database of Systematic Reviews. 9 (9): CD003826. doi:10.1002/14651858.CD003826.pub3. PMID 24030657.
Shih R, Waltzman J, Evans GR (March 2007). "Review of over-the-counter topical scar treatment products". Plastic and Reconstructive Surgery. 119 (3): 1091–5. doi:10.1097/01.prs.0000255814.75012.35. PMID 17312518.
Roques C, Téot L (2008). "The Use of Corticosteroids to Treat Keloids: A Review". The International Journal of Lower Extremity Wounds. 7 (3): 137–145. doi:10.1177/1534734608320786. PMID 18611924.
Jenkins M, Alexander JW, MacMillan BG, Waymack JP, Kopcha R. Failure of topical steroids and vitamin E to reduce postoperative scar formation following reconstructive surgery. J Burn Care Rehabil. 1986 Jul–Aug;7(4):309–312.
Nor, N. M.; Ismail, R.; Jamil, A.; Shah, S. A.; Imran, F. H. (2016-11-25). "A Randomized, Single-Blind Trial of Clobetasol Propionate 0.05% Cream Under Silicone Dressing Occlusion Versus Intra-Lesional Triamcinolone for Treatment of Keloid". Clinical Drug Investigation. 37 (3): 295–301. doi:10.1007/s40261-016-0484-x. PMID 27888448.
"Scar revisions". Archived from the original on 19 January 2012. Retrieved 16 October 2010. Deep cuts need multi-layered closure to heal optimally; otherwise, depressed or dented scars can result
Farris PK. Topical vitamin C: a useful agent for treating photoaging and other dermatologic conditions. Although many people claim that vitamin therapy does in fact help. Dermatol Surg 2005;31:814-818.
Mee, Donna; Wong, Brian (2012-10-01). "Medical Makeup for Concealing Facial Scars" (PDF). Facial Plastic Surgery. 28 (5): 536–540. doi:10.1055/s-0032-1325647. PMID 23027221.
Shin, Thuzar M.; Bordeaux, Jeremy S. (2012). "The Role of Massage in Scar Management: A Literature Review". Dermatologic Surgery. 38 (3): 414–423. doi:10.1111/j.1524-4725.2011.02201.x. ISSN 1076-0512. PMID 22093081.
Cohen, BE; Elbuluk, N (February 2016). "Microneedling in skin of color: A review of uses and efficacy". Journal of the American Academy of Dermatology. 74 (2): 348–55. doi:10.1016/j.jaad.2015.09.024. PMID 26549251.
eschara, Charlton T. Lewis, Charles Short, A Latin Dictionary, on Perseus
ἐσχάρα, Henry George Liddell, Robert Scott, A Greek-English Lexicon, on perseus
Online Etymology Dictionary
Online Etymology Dictionary
Renovo. [1]. Lancet trials in: 11 April 2009 (vol. 373, pages 1264-1274). Lancet commentary by Edward Tredget in: vol 373, pages 1226-1228
"Liver damage 'could be reversed'". BBC News. 27 December 2007. Retrieved 1 January 2008.
'Molecular mechanisms linking wound inflammation and fibrosis: knockdown of osteopontin leads to rapid repair and reduced scarring'
"Gel 'to speed up wound healing'". BBC News. 22 January 2008. Retrieved 23 May 2010. |